Translate this page into:
Rare case of bear mauling injury: Reconstruction using patient specific implants
*Corresponding author: Dr. Kumar Saket, Department of Maxillofacial Surgery, Rajiv Gandhi University of Health Sciences, Bangalore, Karnataka, India. saket0410@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Saket K, Vijapur M, Gour A, Kattimani V. Rare case of bear mauling injury: Reconstruction using patient specific implants. J Health Sci Res. 2025;10:35-9. doi: 10.25259/JHSR_36_2024
Abstract
Traumatic skin injuries, including those from animal bites, pose challenges to emergency centers worldwide. This case involves a 41-year-old male mauled by a sloth bear, sustaining severe facial and scalp wounds. Computed tomography revealed extensive damage, prompting the use of patient-specific implants (PSI) via 3D printing and CAD-CAM technology. The PSI, designed to mirror the healthy side, precisely fits the zygomatic bone, supported by screws. Postoperative monitoring showed no complications after 6 months. Maxillofacial defects, complex due to their functional and aesthetic importance, are difficult to treat. Advances in additive manufacturing (AM) have enabled the creation of custom-made implants such as PSI, offering precise reconstruction. Despite cost implications, the benefits of PSI in enhancing outcomes justify its use in challenging maxillofacial cases, such as those resulting from sloth bear attacks.
Keywords
3D printing
Maxillofacial reconstruction
Patient-specific implants (PSI)
Traumatic skin injuries
Sloth bear attack
INTRODUCTION
Traumatic skin lesions are a substantial concern for emergency care providers worldwide, accounting for around 11 million visits annually.[1] Dog and cat bites are believed to be responsible for one to two million occurrences.[2] Although accurate numbers are unavailable due to a lack of mandatory reporting of such injuries, their significance and consequences should not be overlooked.[1] Dogs, cats, horses, rats, and bears are the animals most commonly recorded to bite people.[3] Bear assaults are prevalent in India, particularly throughout the Himalayan range. All bears are potentially hazardous, unpredictable, and capable of causing significant harm.[2]
CASE REPORT
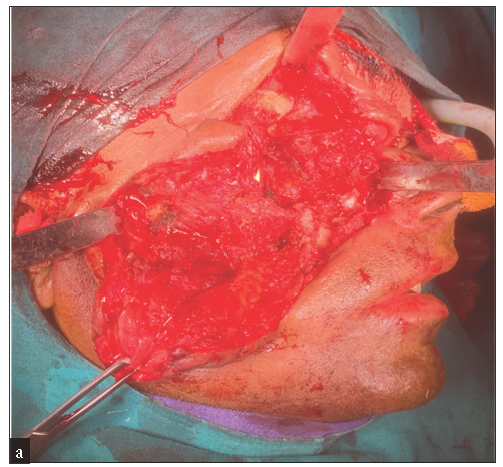
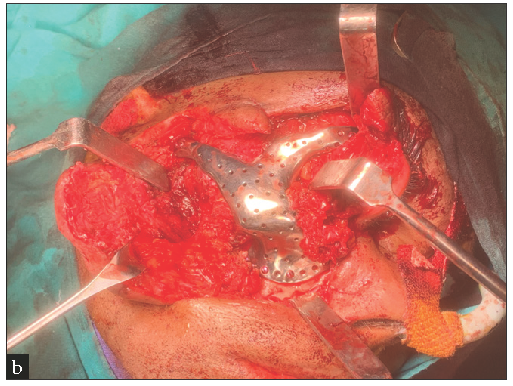
A 41-year-old male patient arrived at KIMS casualty in shock, with lacerations on his face, scalp, and right hand. According to the patient’s relatives, a sloth bear attacked him in the forest of his local hamlet. He was escorted to the community health center where he received first aid and a stay suture was placed. The patient was sent to our department following a 5-hour travel. The patient was hospitalized and transferred to the emergency department, where a preliminary examination revealed wounds on the right side of his face [Figure 1a], orbit [Figure 1b], and both forearms. He suffered a 4 × 3 cm scalp incision on the frontal [Figure 2] and right temporal area. A facial wound of about 4 × 4 cm was seen on the right side of the face, spanning superiorly inferiorly 1 cm from above the left zygomatic arch to 1 cm below the right ear lobe and anterior–posteriorly from the medial canthus of the left eye to 1 cm in front of the tragus of the ear. The damage also affected his right orbital cavity, which seemed to be avulsed. Periorbital edema and ecchymosis, as well as subconjunctival hemorrhage in his right eye, were noted, along with reduced eye movement in the afflicted eye. An anti rabies vaccination was delivered prophylactically with a tetanus vaccine. The wounds were debrided, and bleeding spots were located and hemostasis was accomplished under local anesthesia. The patient was promptly started on intravenous fluid resuscitation using Ringer Lactate and normal saline, as well as broad-spectrum antibiotics. Neurosurgical, orthopedic, and maxillofacial consults were also sought.

- A 41-year-old male mauled by a sloth bear, laceration measuring 4 x 4 cm on the right side of the face.

- Image showing periorbital injury and missing floor of the orbit on the right side.

- Image showing laceration measuring 4 x 3 cms on frontal and right temporal scalp area.
A CT scan revealed a missing right zygoma and the right floor of the orbit, including the zygomatic arch, with no damage to the underlying dura or cerebral structures [Figure 3a, b]. The decision was to employ innovative PSI reconstruction techniques that integrated 3D printing with CAD-CAM.
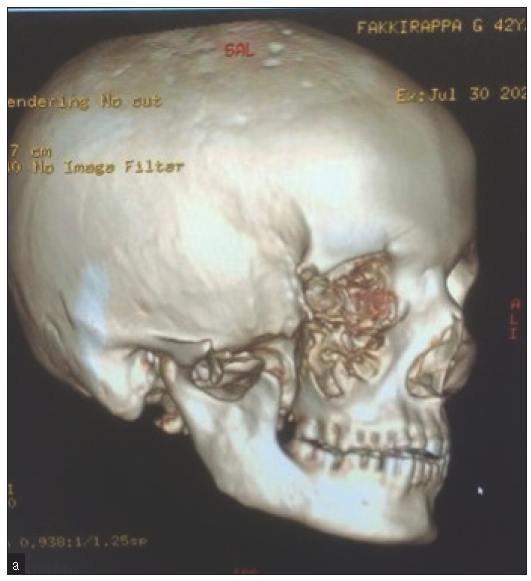
- Computed tomography image showing a missing right zygoma and right floor of the orbit including the zygomatic arch.
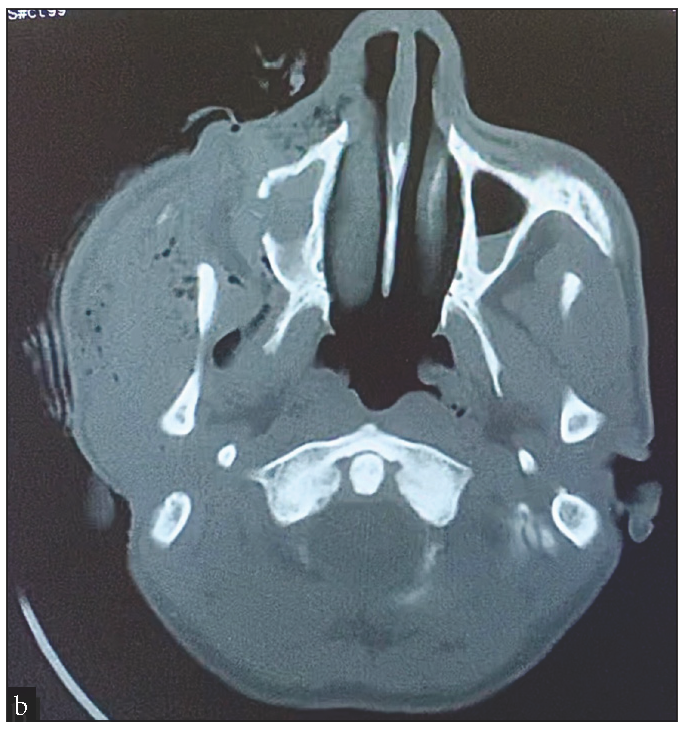
- Computed tomography image showing no damage to the underlying dura or cerebral structures.
A computerized tomography scanner generated a series of tomographic images of the complete skull with a resolution of 0.5 mm. These images were converted from 2D slices into an accurate 3D computer model [Figure 4a], which could then be exported to other design and analysis software as an STL format 3D surface structure. The software was utilized for surface smoothing, hole filling, and quality analysis, aiding in quantifying the changes in zygoma form and symmetry post-surgery. The PSI was created using software capable of generating parametric models that can be easily adjusted based on various factors. It was constructed as a shell with a consistent thickness of 0.5 mm, resembling the unaffected side of the zygomatic complex.
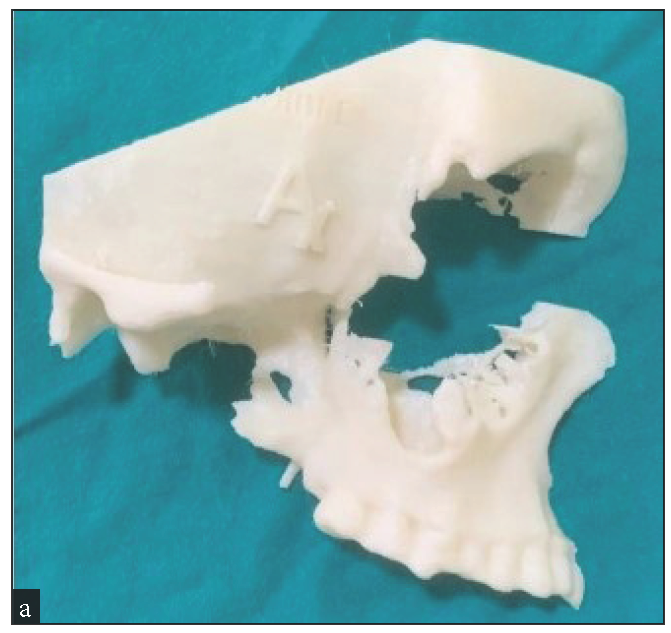
- Image showing 3D computer mode of right zygoma.
The zygoma CAD model was mirrored along a virtual median sagittal plane to establish a symmetrical reference for implant design. The mirrored zygoma CAD model was then modified to create a prototype PSI shape that matched the defect location [Figure 4b]. Screw placement locations were determined based on bone support, and corresponding holes were incorporated into the PSI design to accommodate the screws. The final PSI design was exported in Standard Triangle Language (STL) format, compatible with 3D printers [Figure 4c].

- Preliminary PSI matching the defect area. PSI: Patient-specific implants
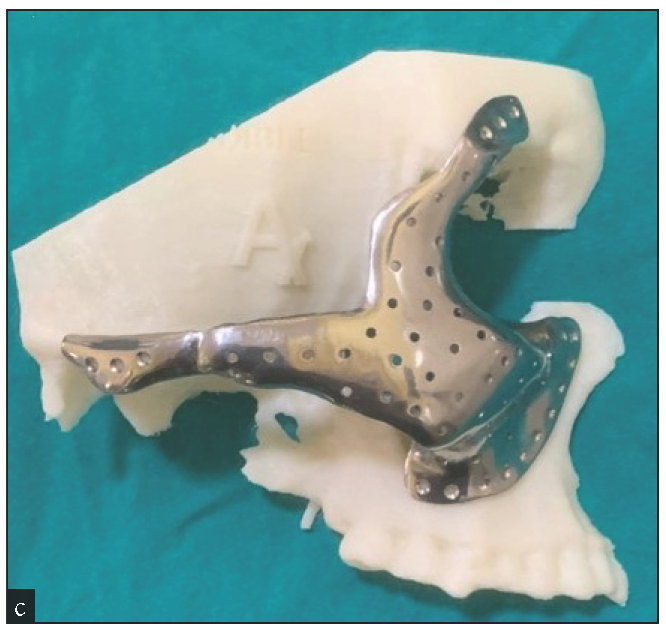
- Image showing the final placement of PSI on a 3D model. PSI: Patient-specific implants
A thorough patient counseling was conducted to highlight the risk and potential consequences of the proposed procedure. The surgical technique, its associated risks, advantages, and available options were thoroughly explained to the patient during counseling. The patient gave his explicit informed consent, guaranteeing that he was aware of the nature of the procedure and that a 3D-printed implant would be used in his reconstruction. The existing laceration exposed the mid face and zygomatic region [Figure 5a] and the PSI was inserted [Figure 5b], fitting snugly into the zygomatic bone on each side. Fixation was carried out with screws of 2 mm diameter and 8 mm length [Figure 5c]. The cornea was covered with a corneal seal, and the lower orbit was formed with PSI to support and raise the eye. No significant boats were impacted.
- Incision was placed from existing laceration.
- Image showing exposed mid-face with PSI placed. PSI: Patient-specific implants
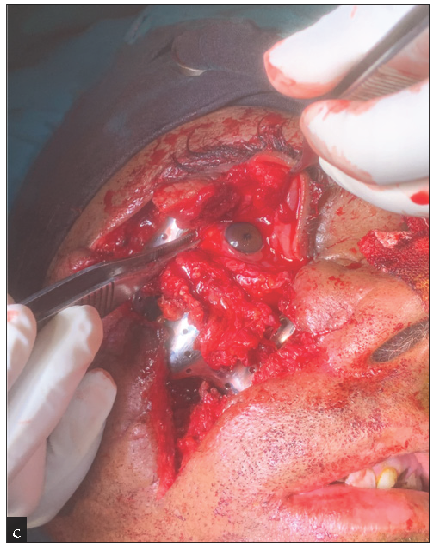
- Fixation done using 2 mm diameter and 8 mm length screws accordingly.
Layer-wise suturing was performed using 5-0 Vicryl and 4-0 Proline [Figure 6], followed by antibiotic treatment. The patient was observed for 6 months with regular follow-ups, and there was no sign of postoperative infection or PSI exposure. The postoperative X-ray revealed that the PSI was properly fitted and positioned.

- Immediate post-op sutured picture.
DISCUSSION
Maxillofacial abnormalities are difficult to cure because they have significant functional, aesthetic, and psychological implications.[3] The anatomical intricacy of this area has further added to the difficulty it poses to all surgeons.[4] Advances in additive manufacturing (AM) technology and 3D imaging have significantly improved the management of maxillofacial abnormalities.[5] This has permitted the production of custom-made PSI that resembles the healthy side to get an acceptable outcome.[6] The main disadvantage of using PSI is its expensive cost, which will undoubtedly force many patients to seek out more cheap alternatives.[7] However, we feel that the numerous benefits of adopting PSI exceed the drawbacks.[8–10]
CONCLUSION
Most surgeons find it difficult to reconstruct maxillofacial deformities because of the region’s complicated structure and the aesthetic and functional consequences the deformities have on patients. The use of prefabricated alloplastic implants and autogenous grafts is frequently linked with resorption, infection, and displacement. Recent technical breakthroughs have resulted in the usage of bespoke computer-designed patient-specific implants (PSIs) in reconstructive surgery. A 3D reconstruction of the zygoma is one of the most difficult procedures in craniofacial surgery because of its complicated architecture, which includes a unique combination of concave and convex surfaces, poor osteogenic capability, and closeness to the maxillary sinus, eye globe, orbit, and cranial base.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)–assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Patient-specific implants for maxillofacial defects: Challenges and solutions. Maxillofac Plast Reconstr Surg. 2020;42:15.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Animal bite injuries to the face: A case report. J Int Oral Health. 2013;5:68-72.
- [PubMed] [PubMed Central] [Google Scholar]
- Use of customized polyetheretherketone (PEEK) implants in the reconstruction of complex maxillofacial defects. Arch Facial Plast Surg. 2009;11:53-7.
- [CrossRef] [PubMed] [Google Scholar]
- Application of patient-specific implants as alternative approach to zygoma defect management—A retrospective study. Ann Maxillofac Surg. 2021;11:91-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Zygoma reconstruction. Oral Maxillofac Surg Clin North Am. 2013;25:167-201.
- [CrossRef] [PubMed] [Google Scholar]
- Computer-assisted therapy in orbital and mid-facial reconstructions. Int J Med Robot. 2009;5:111-24.
- [CrossRef] [PubMed] [Google Scholar]
- 3D modeling, custom implants and its future perspectives in craniofacial surgery. Ann Maxillofac Surg. 2014;4:9-18.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A case report of zygomatic fracture reconstruction: Evaluation with orbital measurements and models registration. Appl Sci. 2023;13:6154.
- [CrossRef] [Google Scholar]
- Reconstruction of maxillofacial bone defects using patient-specific long-lasting titanium implants. Sci Rep. 2022;12:7538.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Recent advances in the reconstruction of cranio-maxillofacial defects using computer-aided design/computer-aided manufacturing. Maxillofac Plast Reconstr Surg. 2018;40:2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






