Translate this page into:
Paecilomyces lilacinus: An Emerging Pathogen
*Email: sabithababy@gmail.com
Abstract
Paecilomyces is a common saprophyte found in air and food and is also associated with many types of human infections. Pneumonia due to Paecilomyces is rare and the clinical manifestations are unspecific. So distinguishing Paecilomyces infection clinically and prompt microbiological identification will help in adminiatering empirical antifungal therapy. We describe a case of atypical pneumonia by Paecilomyces lilacinus in a patient with interstitial lung disease and cor pulmonale. The female patient had breathlessness for over two years and was admitted to hospital as it worsened. Her X-ray revealed right and left ventricular failure. Sputum was sent for fungal bacterial culture and KOH for fungal elements. The Culture on Sabourouds Dextrose Agar grew purecolonies of Paecilomyces.
Keywords
Paecilomyces lilacinus
Pneumonia
Lactophenol Cotton Blue
Sabauraud’s Dextrose Agar
Introduction
Paecilomyces species are generally encountered as common soil saprophytes and a rare airborne contaminant in diagnostic microbiology laboratories1. Literature search reveals majority of the infections caused by paecilomyces among healthy hosts due to endophthalmitis following intraocular lens implantation2. In immuno compromised patients. Paecilomyces lilacinus causes cutaneous infection, catheter related fungaemia and disseminated disease secondary to application of contaminated skin lotions3.
Case Report
A lady aged 56 years with known history of type 2 diabetes mellitus, Chronic Obstructive Pulmonary Disease (COPD) and hypothyroidism presented to our hospital with complaints of productive cough and breathlessness for the past two days.
The patient had history of breathlessness for two years which had aggravated in the last two days. Breathlessness was gradual in onset, aggravated by dust and relieved by medication. There was no history of haemoptysis.
On general physical examination her vitals were stable. There were mild pallor and clubbing. There was no cyanosis, lymphadenopathy or edema. She was conscious, oriented and cooperative. Examination of respiratory system revealed wheeze, polyphonic rhonchi, inspiratory and expiratory crepitations all over her chest.
Chest X-ray showed features of left and right ventricular failure. Echocardiogram detected left and right ventricular dysfunction with moderate pulmonary artery hypertension. Ejection fraction was 55%. Based on the above investigations, a diagnosis of interstitial lung disease with cor pulmonale was made. Empirical therapy was started with Amoxyclav and clarithromycin. She was also started on Oxygen.
Also, with suspicion of atypical pneumonia, sputum was sent for fungal staining and culture. After three days of admission, her condition deteriorated clinically, she complained of headache became drowsy. She was shifted to the ICU. Arterial blood gas analysis was carried out. Findings were suggestive of CO2 retention. Ryles tube was put and she was started on continuous positive airway pressure.
Microbiology Work Up
Sputum gram stain showed normal bacterial flora. Acid fast staining did not show any acid fast bacilli. Wet mount with KOH showed hyaline, septate hyphae. Sputum was inoculated into Blood agar, Mac Conkey agar and Sabouraud’s Dextrose Agar (SDA). Bacterial culture grew normal flora. After three days, slightly lilac coloured granular colonies were seen growing on SDA. Within one week the colour of the colonies turned to a darker shade of vinaceous. (Figure 1).
- Lilac coloured colonies of Paecilomyces lilacinus.
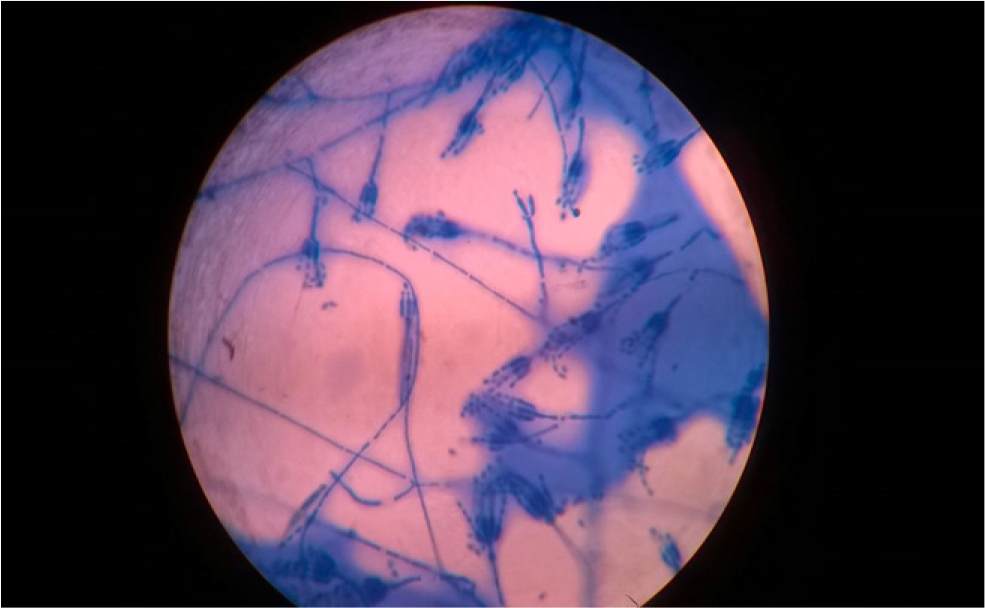
LPCB (lactophenol Cotton Blue) mount from the colonies produced hyaline septate hyphae and elongated, tapering phialides with several elliptical conidia. (Figure 2). Conidiogenous cells were branched, cylindrical, and loosely clustered, tapering gradually to a fine point. The conidia were globose and ellipsoidal and were produced endogenously to form a very long chain. Based on the colony morphology and microscopy findings, the isolate was identified as Paecilomyces lilacinus. The vinaceous pigmentation of the colonies and a careful study of the microscopical features are the most useful criteria for distinguishing this fungus from common contaminants, e.g., Penicillium, which shows a similar arrangement of the fertile hyphae, or from other more common pathogenic fungi, e.g., Aspergillus and Candida spp.
The patient was given oral fluconazole and posaconazole syrup. The patient improved clinically and was eventually discharged after five days. Further review after 2 weeks were uneventful. Complete cure was achieved during the follow-up period of 2 months.
-
Paecilomyces lilacinus hyaline septate hyphae with elongated, tapering phialides with several elliptical conidia.
Discussion
During the past decade, hyalohyphomycosis has been increasingly recognised. This could be because of 1. Increased awareness among clinicians 2. Improved diagnostic tools and 3. Increased host susceptibility4.Risk factors for non Aspergillus hyaline mold infections are similar to those for invasive aspergillosis. These environmental molds enter humans by inhalation or by cutaneous inoculation.
Presence of Paecilomyces have been considered as contaminant, however several cases of infection in humans and animals have been reported. The rare case reports in humans involve corneal ulcer, keratitis, and endophthalmitis following extended wear contact lens use or ocular surgery5.
Also Paecilomyces predominanly cause diseases in patients immunocompromised from haematopoietic cell malignancies, diabetes, HIV/AIDS, chronic granulomatous disease and by corticosteriods. It has also been implicated as the cause of cell mediated granulomatous allergic alveolitis (without pneumonia) in individuals living in proximity to decaying wood6.
In the present case, the patient had diabetes and hypothyroidism. The fungus Paecilomyces is a soil saprophyte and this patient may have acquired the infection during outdoor work when the fungal spores were inhaled. Posaconazole, the novel triazole demonstrated effectiveness in treatment of pneumonia from Paecilomyces in our patient. The clinical manifestations of this fungal infection are unspecific and include fever, pleuritic chest pain, productive cough, and dyspnea. Hilar lymphadenopathy, nodules, confluent and patchy opacities, and cavitary lesions are the most common imaging abnormalities.
Paecilomyces variotii and Paecilomyces lilacinus are the two species most frequently associated with human disease. Other species reported to infect humans rarely include Paecilomyces marquandii and Paecilomyces javanicus7. Paecilomyces lilacinus, show poor susceptibility to amphotericin B, itraconazole, and echinocandins, while Paecilomyces variotii shows a different susceptibility pattern, being susceptible to most antifungal agents apart from voriconazole. So determination of the precise specie of Paecilomyces is important for the appropriate management and treatment of these infections.
Paecilomyces lilacinus has been reclassified under the genus Purpureocillium as the genus Paecilomyces was not monophyletic. Genus Purpureocillium contains the single species Purpureocillium lilacinum8. P. lilacinum may be entomopathogenic9,10, mycoparasitic11, saprophytic, nematophagous as well as an emerging human pathogen. A peculiar characteristic of P. lilacinus is its ability to sporulate in infected tissue, can be helpful in the diagnosis of these infections. This type of sporulation, called ‘adventitious’ sporulation, involves the production of reproductive structures similar to those observed in vitro, i.e., phialides and conidia.
There are limitations for conventional diagnostic methods namely culture due to low sensitivity and slow turnover time. However, culture and microscopy remain the cornerstone of diagnosis. Recently, in11 described a precise molecular method for the identification of Paecilomyces species based on the sequence of the intergenic transcribed spacer regions 1 and 2 (including the 5.8S rDNA) and a part of the beta-tubulin gene12. A review of the published literature identified 119 reported cases of human infection by P. lilacinus between 1964 and 2004. Most were cases of oculomycosis (51.3%), followed by cutaneous and sub-cutaneous infections (35.3%), and a smaller group of miscellaneous infections (13.4%). Lens implantation is the most frequent predisposing factor for oculomycosis. Cutaneous and sub-cutaneous infections occur mainly in solid organ and bone marrow transplant recipients, although surgery and primary or acquired immunodeficiency are also relevant predisposing factors. Infections in apparently immunocompetent patients have also been reported. Surgical debridement combined with antifungal drug therapy, or the correction of predisposing factors, such as neutropenia, are usually required to obtain improvement13.
Conclusion
The present case report provides us with an insight to consider opportunistic pathogens like Paecilomyces causing serious infections in immunocompromised patients and increased awareness about this fungus will help in prompt diagnosis and better patient care in future. This experience emphasizes the potential pathologic nature of this fungus when immunity is compromised by poorly controlled diabetes and other underlying factors.
References
- Fungal endophthalmitis following intraocular lens implantation. Archives of Ophthalmology. 1980;98(6):1025.
- [CrossRef] [PubMed] [Google Scholar]
- Outbreak of Invasive Mycoses Caused by Paecilomyces lilacinus from a Contaminated Skin Lotion. Annals of Internal Medicine. 1996;125(10):799.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic invasive fungal rhinosinusitis by Paecilomyces variotii: A rare case report. Indian J Med Microbiol. 2016;34:103-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pneumonia and lung infections due to emerging and unusual fungal pathogens. Seminars in Respiratory and Critical Care Medicine. 2011;32(6):703-16.
- [CrossRef] [PubMed] [Google Scholar]
- Guide to Clinically Singnificant Fungi Baltimore, Md, USA: Willians and Wilkins; 1998.
- [Google Scholar]
- Identification and taxonomy of some entomopathogenic Paecilomyces spp (Ascomycota) isolates using rDNA-ITS Sequences. Genetics and Molecular Biology. 2006;29(1):132-6.
- [CrossRef] [Google Scholar]
- Isolation of Paecilomyces lilacinus (Thom) Samson (Ascomycota: Hypocreales) from the Chagas disease vector. Triatoma Infestans Klug Hemiptera: Red... -PubMed - NCBI. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17123036
- [Google Scholar]
- Nematophagous fungus Paecilomyces lilacinus (Thom) Samson is also a biological agent for control of greenhouse insects and mite pests. Bio Control. 2007;52(4):547-58.
- [CrossRef] [Google Scholar]
- Hydrolytic enzymes secreted by Paecilomyces lilacinus cultured on sclerotia of Aspergillus flavus. Appl Microbiol Biotechnol. 1993;39(1):99-103.
- [CrossRef] [Google Scholar]
- Identification of Paecilomyces varioti in clinical samples and settings. Journal of Clinical Microbiology. 2010;48(8):2754-61.
- [CrossRef] [PubMed] [Google Scholar]
- Paecilomyces variotiias an emergent pathogenic agent of pneumonia. Case Reports in Infectious Diseases. 2013;2013:1-3.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical manifestations, treatment and outcome of Paecilomyces lilacinus infections. Clinical Microbiology and Infection. 2006;12(10):948-60.
- [CrossRef] [PubMed] [Google Scholar]






