Translate this page into:
Complications profile following regional anesthesia: Comparative analysis between ankle and unilateral spinal blocks for foot surgery
Corresponding author: Dr. Bashir Garba Aljannare, Department of Anesthesia and Intensive Care, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria. bashiraljannare@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Aljannare BG, Khalid A, Abdulrahaman A, Bello IG. Complications profile following regional anesthesia: Comparative analysis between ankle and unilateral spinal blocks for foot surgery. J Health Sci Res. 2024;9:37–42. doi: 10.25259/JHSR_42_2023
Abstract
Objectives
This study aims to compare the complications profile between ankle block and unilateral spinal block for foot Surgeries. Ankle block is expected to provide minimal intraoperative and postoperative complications compared to unilateral spinal block following foot surgeries.
Material and Methods
Fifty adult patients scheduled for elective foot surgeries that met the inclusion criteria were enrolled in the study. They were assigned into two groups of 25 each as they came, group A (ankle block) and group S (unilateral spinal block). Group A had surgery under the ankle block using 4 ml of 0.5% plain bupivacaine to block each nerve. In contrast, group S had surgery under a unilateral spinal block using 3 ml of 0.5% heavy bupivacaine. The complications were observed and recorded.
The data obtained were analyzed using Statistical Package for Social Sciences version 25.0 and were presented using relevant proportions, tables, and figures. Statistical association tests were performed with a confidence level of 95%, and a p-value of less than 0.05 was taken as significant.
Results
The intraoperative complications observed between the two groups; three patients (12%) had nausea for group S while two patients (8.7%) had nausea from group A, two patients (8%) had vomiting from group S while one patient (4%) from group A had vomiting, three patients (12%) had bradycardia from group S and one patient (4%) had bradycardia from group A, three patients (12%) from group S had hypotension while no patient had hypotension from group A.
The postoperative complications between the two groups; 2 (8%) patients had nausea from group S while only one patient (4%) had nausea from group A, Only 1 (4%) patient had vomiting from group S and one patient (4%) had vomiting from group A. Only two patients (8%) had urinary retention from group S, while no patients from group A had urinary retention. No patient had a postural puncture headache or shivering from group S.
Conclusion
Ankle block is associated with minimal complications compared to unilateral spinal block.
Keywords
Complications
Ankle block
Unilateral spinal block
Foot Surgeries
INTRODUCTION
Anesthesia is a critical consideration for patients undergoing any form of surgery, whether minor or major. Several anesthetic techniques are available for surgery. However, the most prevalent anesthetic techniques are general and conventional neuraxial anesthesia. These common techniques have associated complications and side effects that make them less than ideal for patients coming for surgery. The side effects of general anesthesia include myocardial depression, postoperative nausea and vomiting, cardiovascular and respiratory depression, sore throat, and myalgia, amongst other things. On the other hand, postoperative backache, hypotension, urinary retention, and post-dural puncture headache can complicate neuraxial spinal anesthesia and result in delayed hospital discharge.[1]
It has been established that inadequate postoperative pain relief prolongs postoperative recovery and length of hospital stay and increases the cost of care, especially in the poverty-endemic part of the world.[2]
The foot is one of the essential parts of the body that faces many problems, such as trauma, strain, infections, and other pathological conditions. Soft tissue foot injuries, debridement, dislocations to the toes and digits, fractures, traumatic and non-traumatic amputations, abscesses drainage from diabetic foot, and rarely soft tissue tumors are common indications for foot surgeries.[3] Surgeries for most of these cases are done under general anesthesia and conventional spinal anesthesia in most peripheral hospitals, no matter how short the procedure may be. This imposes a greater risk on the patients and exposes them to the attendant complications of general anesthesia and conventional spinal anesthesia. These surgeries can be performed under the unilateral spinal and peripheral nerve blocks, thereby avoiding these complications.[4]
Regional anesthesia for foot surgeries is relatively simple, safe, effective, and affordable. It is also devoid of major complications.[5] These techniques can be performed with minimal gadgets or expertise, even in developing countries. On the other hand, the ankle block is expected to have fewer complications than the unilateral subarachnoid block for foot surgeries. These two modalities are used in our routine practice, but their associated complications have not been studied. Therefore, this study aims to assess the complications associated with regional anesthesia, emphasizing ankle block and unilateral subarachnoid block for foot surgeries. Ankle block is expected to have fewer complications when compared to unilateral spinal block for foot surgeries.
This study’s outcome will help encourage using alternative anesthetic techniques to general anesthesia for foot surgeries. It will also contribute to our subregion’s limited reference database for peripheral nerve blocks.
Material and Methods
This is observational hospital-based study of American Society of Anesthesiologists (ASA) I or II patients aged between 18 and 60 years scheduled for elective foot surgery was conducted at our Teaching Hospital in Northwestern Nigeria from April 2020 to October 2020. Approval for the study UDUTH/HREC/2019/No.803 was obtained from our hospital’s research and ethics committee.
After written informed consent, fifty patients with ASA physical status I and II, between the ages of 18 and 60 years, scheduled to undergo elective foot surgeries under regional anesthesia were included in the study.
Any patient who refused the procedure, a patient with a history of drug allergy, infection at the site of the block, coagulopathy, a patient on anticoagulants and distorted anatomy of the foot or spine, and a patient with compromised vascular supply to the foot was excluded from the procedure.
The sample size was determined using the figures from a similar study by Urafalioglu et al [6] and using an effect size based on the following formula,
Where;
N = minimum sample size per group
a1 = Standard deviation of ankle block group = 0.48
b2 = Standard deviation of unilateral subarachnoid block group = 1.27
Z1 = z score corresponding to 95% level of significance = 1.96
Z2 = z score corresponding to 80% statistical power of study = 0.84
M1 = Mean visual analogue scale (VAS) score in ankle block group = 1.20
M2 = Mean VAS score in unilateral subarachnoid block group = 2.37
Therefore: N = (1.272 + 0.482) (1.96 + 0.84)2/(2.37 - 1.20)2 = 10.53
10% attrition was made for patients who might drop out of the study. Therefore, 10% of 10.53 = 1.05, and the total sample size, 10.53 + 1.05 = 11.58, approximated to 12.
To improve from the previous study, an effect size was added using the following formula[7] of effect size calculation as follows: nf = n/1 + n/N
Where, nf = required sample size if the target population is < 10,000
n = calculated sample size from the previous study = 12
N = estimated target population = 85, i.e., number of foot surgery cases in a year.
Effect size, nf = 12/1+12/85 = 11. Sample size = 12 + effect size (11)
Therefore, the minimum sample size per group = 23
However, 25 patients were used for each group. Fifty ASA physical status I or II patients were randomly assigned into groups A and S. Group A represents the ankle block group, while group S represents the unilateral spinal block group.
All the patients were visited a day before the surgery, during which a detailed pre-anesthetic evaluation was done, the study protocol was explained to the patients, and written informed consent was obtained from these patients. They were instructed to fast according to the fasting guidelines, and routine laboratory investigations were reviewed.
The materials used for these blocks consist of sterile gloves, different sizes of syringes with 25 G hypodermic needle for skin infiltration, 1% lidocaine, 0.5% plain bupivacaine, 0.5% heavy bupivacaine, sterile spinal pack, drapes, and size 25 G spotted spinal needles. All necessary equipment and drugs needed for resuscitation and conversion to general anesthesia were kept ready in case of block failure or a toxic reaction to the local anesthetic agent during the procedure.
The following equipment were used for the study: A pulse oximeter (CAS M. California, USA) to monitor pulse rate and peripheral oxygen saturation, a non-invasive blood pressure cuff to monitor blood pressure using a Dash 4,000 multiparameter (SAKOMED, Laguna Niguel, USA) monitor, a stopwatch to measure onset and duration of sensory block.
On arrival at the operating room, intravenous access on the hand was secured using a wide-bore cannula for fluid administration. Standard monitoring, including peripheral oxygen saturation (SpO2), non-invasive blood pressure (NIBP), and Electrocardiography (lead II and V5) were set up. The baseline readings were obtained and recorded at a 5-minute interval throughout the procedure.
Ankle block was performed by placing the patient in the supine position and keeping the pillow underneath the lower leg to improve access to all five nerves, namely, the Deep peroneal nerve, superficial peroneal nerve, saphenous nerve, posterior tibial nerve, and the sural nerve. The aseptic technique was ensured, and 4 ml of 0.5% plain bupivacaine was deposited after test aspiration to block each of the abovementioned nerves.
A unilateral spinal block was administered by placing the patient in a lateral decubitus position depending upon the site of the surgery and under the aseptic technique, using a low dose (3 ml) of 0.5% heavy bupivacaine after obtaining free flow of cerebrospinal fluid from the intervertebral space at third/ fourth lumbar space (L3/L4).
The vital signs, pulse rate, and blood pressure were observed and recorded at 5-minute intervals throughout the procedure. The monitoring of vital signs continued in the post-anesthesia care unit and at 1st, 2nd, 4th, 8th, 12th, and 24th postoperatively.
The baseline pulse rate and blood pressure were measured and recorded. This monitoring continued throughout the intraoperative period until patients were transferred to the recovery room in the surgical ward postoperatively at the 1st, 2nd, 4th, 8th, 12th, and 24th hours.
The undesirable side effects were managed accordingly: bradycardia with an intravenous dose of Atropine 0.5 mg, hypotension with intravenous fluid, and 5 mg intravenous ephedrine. Patients desaturated to less than 95% were given supplemental oxygen via face mask. In this study, two patients had failed ankle block, and these patients were converted to conventional subarachnoid block and therefore excluded from the study. Only data from patients well-oriented in person, place, and time were considered for statistical analysis.
STATISTICAL ANALYSIS
Statistical analysis of data obtained from the study was performed electronically using Statistical Package for the Social Sciences (SPSS) version 25. The results obtained were expressed as mean ± SD except where stated otherwise.
Demographic and postoperative data differences between the two groups were sorted out, and variables were analyzed with the unpaired Student’s t-test to ensure a normal distribution. The P-value £ 0.05 was considered significant.
RESULTS
Fifty patients with ASA physical status I and II, between the ages 18 and 60 years, with a mean age of 37.2 and a standard deviation of 11.3, were involved in this study.
The differences in demographic data, age, sex, weight, and ASA classification were comparable and statistically insignificant in both groups [Table 1].
| Group A (n = 23) Mean (±SD) | Group S (n = 25) Mean (±SD) | P-value | |
|---|---|---|---|
| Age (years) | 38.52 (±11.66) | 35.96 (±10.83) | 0.425 |
| Sex (M, F) | 14 (60.9%), 9 (39.1%) | 16 (64%), 9 (36%) | 0.564 |
| Weight (Kg) | 65.56 (±8.07) | 63.96 (±9.92) | 0.535 |
| ASA Status I/II | 13 (56.5%), 10 (43.5%) | 17 (68%), 8 (32%) | 0.382 |
P £ 0.05, the difference is statistically significant; ASA: American Society of Anesthesiologists.
The total number of complications observed among all the patients (n = 50): Intraoperatively, five patients (10%) had nausea, three patients (6%) had vomiting, four patients (8%) had bradycardia and three patients (6%) had hypotension. Postoperatively, three patients (6%) had nausea, two patients (4%) had vomiting and two patients (4%) had urinary retention. No patients had shivering, post-dural puncture headache (PDPH), bradycardia, or hypotension during the postoperative period.
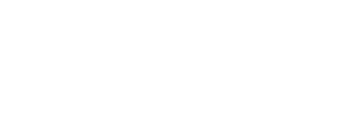
The intraoperative complications observed between the two groups (n = 25); three patients (12%) had nausea for group S while two patients (8%) had nausea from group A, two patients (8%) had vomiting from group S while one patient (4%) from group A had vomiting, three patients (12%) had bradycardia from group S and one patient (4%) had bradycardia from group A, three patients (12%) from group S had hypotension while no patient had hypotension from group A.
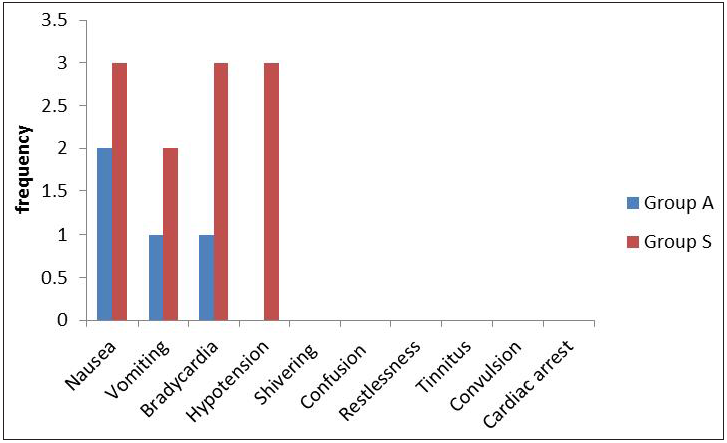
The postoperative complications between the two groups (n = 25); two patients (8%) had nausea from group S while only one patient (4%) had nausea from group A, Only one patient (4%) had vomiting from group S and one patient (4%) had vomiting from group A. Only two patients (8%) had urinary retention from group S, while no patients from group A had urinary retention. No patient had a postural puncture headache or shivering from group S. This is illustrated more in Figures 1 and 2.
- Intraoperative complications between ankle block and unilateral spinal block.
- Postoperative complications between ankle block and unilateral spinal block.
Complications related to bupivacaine toxicity, such as confusion, restlessness, tinnitus, convulsion, and cardiac arrest, were looked out for, but none were recorded in this study.
DISCUSSION
The common side effects of peripheral nerve block are incomplete block, direct nerve injury, hematoma, infection, and the risk of intravenous administration of local anesthetics agent.[8] In this study, two patients had failed ankle block, and these patients were converted to conventional spinal and, therefore, exempted from the study. Hajek et al. [9] reported superficial peroneal nerve and sural nerve injuries in 3 patients out of 157 patients, representing (1.9%) who were anesthetized with continuous popliteal nerve block for hallux valgus surgeries. Despite the small chances of nerve injuries in the peripheral block, patients should be informed about such side effects.
The toxicity related to local anesthetic agents can be prevented by using a safe dose of local anesthetic agents and testing aspiration before administration of local anesthetic agents. In this present study, these preventive measures were ensured. The correct identification of nerve landmarks can avert the problems of incomplete nerve block and direct nerve injury.
Intraoperatively, three patients (12%) had nausea, two patients (8%) had vomited in group S, while two patients (8.7%) had nausea, and only one (4.3%) patient had vomited in group A. Three patients (12%) had bradycardia, and three patients (12%) had hypotension in group S, while in group A, only one patient (4.3%) had bradycardia and no patient had hypotension.
Postoperatively, two patients (8%) had nausea, and 1 patient (4%) had vomited in group S. In group A, only 1 patient had nausea and vomiting. In group S, two patients (8%) had urinary retention requiring catheterization, and no patient had urinary retention in group A. Similar to our findings, Singh et al. [10] and Urfalioglu et al. [6] also recorded nausea, vomiting, bradycardia, and hypotension. In this study, no patient had a post-dural puncture headache because a dura-cutting spinal needle (Quincke) was not used. Instead, a sprotte spinal needle was used. This is similar to the finding in a study by Krobot and colleagues.[11] In their study, no patient had a post-dural puncture headache. However, in contrast to their finding, several studies [6,10] observed some patients with post-dural puncture headache in group S as a complication. This is because a dura-cutting spinal needle (Quincke) was used, possibly responsible for post-dural puncture headache.
In a related study, Jeon and colleagues [12] studied forty patients who had foot surgery; these patients were randomly divided into popliteal nerve block and conventional spinal block, and a significant complication of shivering was observed. However, in this study, shivering was not observed. This may be because the unilateral spinal block was used in this present study, and they used a conventional spinal block.
This study had no complications related to bupivacaine toxicity, such as confusion, restlessness, tinnitus, convulsion, and cardiac arrest.
Ahmed et al. [13] reported bradycardia and hypotension, which were reported by Singh et al. [10] only in two patients. The reported bradycardia and hypotension lasted only a few seconds and resolved spontaneously without any intervention. This emphasizes the need for close and continuous monitoring during surgery and in the post-anesthesia care unit (PACU). Anticholinergic drugs such as atropine and vasopressors must be available in operating and post-anesthesia care units when doing procedures under the ankle or spinal block. These anticholinergic and vasopressors should be administered when needed to prevent the adverse effects of bradycardia and hypotension, as reported by Urfalioglu et al.[6]
In this study, most patients who had surgeries due to open wounds to the foot also suffered from hypertension and diabetes mellitus as comorbidity. Therefore, in such patients, the spinal block might affect the hemodynamic values more than the ankle block and pose a greater risk than the ankle block. For this reason, an ankle block is preferable to a subarachnoid block as an anesthetic technique of choice for foot surgeries in these groups of patients.
Intraoperative nausea and vomiting or postoperative nausea and vomiting are important complications because the spinal block is widely used. The underlying mechanism of nausea and vomiting is mainly due to hypotension due to sympatholysis during the neuraxial block. It could also be due to bradycardia owing to an increased vagal tone associated with the subarachnoid block. Hypotension can be prevented with adequate preloading with intravenous crystalloids. It can be treated with intravenous fluids and vasopressors. Intravenous atropine can be used to treat bradycardia. Intraoperative nausea and vomiting and postoperative nausea and vomiting can be treated with intravenous metoclopramide, Ondansetron, and droperidol.
PDPH is a major complication of neuraxial anesthesia. It was described by August Bier in 1899. The exact mechanism is not clear. However, it is postulated to be due to reduced cerebrospinal fluid (CSF) pressure due to loss of CSF in the epidural space through the dural puncture site. The decrease in CSF creates a loss of the cushioning effect normally provided by intracranial fluid. The resulting traction placed on the intracranial pain-sensitive structures elicits pain. Also, with a sudden drop in cerebrospinal fluid pressure, vasodilation of the intracranial vessels occurs to maintain a constant intracranial volume, resulting in a pathophysiology similar to a vascular headache—the beneficial effects of vasoconstrictor drugs such as caffeine and theophylline in PDPH support this mechanism. The type and size of the needle are also important factors in PDPH. The cutting needles (Quincke needles) are associated with a higher incidence of PDPH than blunt or pencil-point needles (Sprotte and Whitacre needles). The conservative treatment includes bed rest and hydration. The epidural saline and blood patch are the definitive treatment for post-dural puncture headache.
LIMITATIONS
The small sample size and being a single-center study were the limitations of this study. There is a need for a large, multi-center study on this research area in the future to validate the findings of this study. Ankle block is a superficial block and purely sensory. The patient will still be able to move their toe and foot. It requires at least 3 separate injections. Placing an ankle block is uncomfortable. The patient may require conscious sedation for analgesia and amnesia to supplement the block.
CONCLUSION
Ankle block is associated with fewer complications when compared to unilateral spinal block for foot surgeries. Ankle block allows the patient to have surgery while awake, provides good postoperative pain relief, and reduces the use of systemic intravenous or intramuscular opioids and their side effects.
Acknowledgment
We sincerely thank all the patients who participated in this study and the staff of our teaching hospital, too numerous to mention, who supported this study.
Ethical approval
The authors declare that they have taken the ethical approval and the approval number is UDUTH/HREC/2019/No.803.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Muric PM. Pharmacoeconomics of intravenous regional anesthesia versus general anesthesia for outpatient surgery. Can J Anesth. 1997;44:1152-6.
- [Google Scholar]
- Peripheral nerve block, clinical Anesthesiology. In: New York Lange Medical Book (4th ed). 2006. p. :906-20.
- [Google Scholar]
- A comparative study between unilateral spinal anesthesia versus ultrasound combined femoro-sciatic nerve block for lower limb surgery. Med. J. Cairo Univer. 2019;87:3059-68.
- [Google Scholar]
- Bupivacaine Anesthesia and Intensive care A-Z an encyclopaedia of principle and practice. (5th ed). Britain: Butter mouth Heinman; 2014. p. :360-5.
- [Google Scholar]
- Comparison of peripheral nerve block, spinal anesthesia and general anesthesia for ambulatory surgery of lower limb. Novel medicus. 2012;8:75-80.
- [Google Scholar]
- A Comparison of ankle block and spinal anesthesia. Int J Clin Exp Med. 2015;15:19388-93.
- [Google Scholar]
- Sample size calculations: Basics principles and common pitfalls. Nephrol Dial Transplant. 2010;25:1388-93.
- [Google Scholar]
- Peripheral nerve block for anesthesia in patients for knee arthroplasty. Korean J Anesthesiol. 2012;62:403-4.
- [Google Scholar]
- Neuropathic complications after 157 procedures of continuous popliteal nerve block for hallux valgus surgery. A retrospective study. Orthopaedic trauma. 2012;98:327-33.
- [Google Scholar]
- Comparative Analysis of Unilateral spinal block with Ankle block for elective foot surgery. Int J Med and Dent Sci. 2016;5:1150-5.
- [Google Scholar]
- Comparison of unilateral spinal block and popliteal sciatic nerve block in elderly undergoing transmetatarsal amputation. Eur J Anaesthesiol. 2012;29:121-5.
- [Google Scholar]
- Popliteal Sciatic nerve block versus spinal block for foot surgery. Korean J Anesthesiol. 2013;64:321-6.
- [Google Scholar]
- Femoral nerve block versus spinal anesthesia for lower limb peripheral vascular surgery. Alex J Anaesth Intensive Care. 2016;9:44-50.
- [Google Scholar]