Translate this page into:
Scrotal calcinosis cutis an unrelated finding in benign prostatic hyperplasia patient, is treatment sine qua non? A case report
* Corresponding author: Dr. Abdullahi Khalid, Department of Surgery, Tetfund Centre of Excellence in Urology and Nephrology, Institute of Urology and Nephrology, Usmanu Danfodiyo University and Teaching Hospital, Sokoto, Nigeria. kalabduka@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Khalid A, Obadele OG, Bello U, Haruna UK, Abdulwahab-Ahmed A. Scrotal calcinosis cutis an unrelated finding in benign prostatic hyperplasia patient, is treatment sine qua non? A case report. J Health Sci Res. 2024;9:85-8. doi: 10.25259/JHSR_29_2023
Abstract
Calcinosis cutis is a reactive and nonmalignant lesion characterized by solitary or multiple cutaneous nodules that can affect different parts of the body including the scrotum among other structures. Treatment is often sought because of cosmesis, itching, or pain. Despite this, it remains unclear or unimaginable why patients will be reluctant to accept treatment in the face of disfigurement. Several reasons have been documented, but the fear of genital mutilation from open surgical intervention is an unfamiliar reason advanced by the index case for declining open surgical intervention. Its diagnosis requires careful clinical evaluation and is confirmed by lesional biopsy for histological confirmation.
This is a case of a 50-year-old trader who presented to our facility with a 35-year history of multiple, painless scrotal nodules and difficulty in passing urine for six months’ duration. He was diagnosed with benign prostatic hyperplasia (BPH) with the indication for surgical therapy and idiopathic scrotal calcinosis cutis. He consented and had endoscopic therapy for benign prostatic hyperplasia (BPH) but was reluctant to open surgical intervention for idiopathic scrotal calcinosis cutis despite disfigurement because of the fear of genital mutilation.
The current treatment options include follow-up observation, medications, cryotherapy, laser, and surgical excision, depending on the patient’s choice, availability, and surgical expertise. The surgical option is often favored and encouraged due to its associated reduced chances of recurrence. Therefore, it is pertinent to respect the patient’s opinion and should override other considerations in clinical practice. The lesson herein can assist other clinicians in avoiding justifiable medical litigations, hence, the need for this case report and a review of the literature.
Keywords
Idiopathic
Scrotum
Calcinosis Cutis
Treatment
Case report
INTRODUCTION
Calcinosis cutis is a reactive condition characterized by solitary or multiple cutaneous nodules that can affect different parts of the body including the scrotum among other structures. It is categorized into five principal types: idiopathic, dystrophic, calciphylaxis, metastatic, and iatrogenic.[1] Idiopathic calcification does not involve underlying tissue damage or abnormal laboratory values and includes tumoral calcinosis, subepidermal calcified nodules, and scrotal calcinosis. Idiopathic scrotal calcinosis was first described by Lewinski[2] in 1883. This pathology is usually of a long-standing duration before it comes to the attention of an attending clinician. Moreover, it has neither been documented to be a premalignant condition nor undergo malignant transformation.[3] They are, at times, discovered during routine clinical examinations when patients present with unrelated complaints.
The common concerns why patients with this disease seek medical consultation and treatment include cosmesis, associated pain, or itching. Currently, surgery remains the only curative option. Despite this, it remains unclear why patients will be reluctant to accept treatment. Some probable reasons why a patient could decline its treatment range from the absence of associated distressful symptoms to disregard for cosmesis based on the individual’s socioeconomic, cultural, and spiritual background as well as geographical location. The other reasons include fear of future sexual dysfunction, impaired quality of life, reduced self-esteem, and the development of complications. Also, the available curative treatment option can be regarded as invasive.[4] The index patient had endoscopic treatment for BPH but was reluctant to receive treatment for scrotal calcinosis despite disfigurement because of the fear of genital mutilation. This is a report on the case of a BPH patient with scrotal calcinosis cutis who declined surgical treatment despite disfigurement and a review of the literature.
CASE REPORT
This is a 50-year-old trader who presented to our facility with a 35-year history of multiple, painless scrotal nodules and difficulty in passing urine for six months’ duration. The nodules gradually increased in size and number to the current state. There was no history of discharge, ulcerations, or infection related to the scrotal lesions. He had a 6-month history of voiding and storage of lower urinary tract symptoms (LUTS) that waxed and waned culminating in acute urinary retention, which was successfully relieved by successful urethral catheterization. He was placed on medical treatment for BPH but failed a trial of micturition without a catheter. There were no remarkable medical comorbidities, family and psychosocial history of note. There were no associated past interventions or use of medications such as immunosuppressive drugs.
He was observed to have multiple, firm, nontender, subcutaneous nodules studded within the scrotal wall and an enlarged prostate with benign features. The laboratory auxiliary tests— blood and urine, including serum calcium, phosphorous, and parathormone levels—were within normal limits. The serum PSA was 5.8 ng/ml. The transabdominal ultrasound scan revealed a prostate volume of 76 ml with intravesical prostatic protrusion of 21 mm. He was counseled and had bipolar transurethral resection of the prostate (bi-TURP) and a biopsy of scrotal lesions [Figure 1]. The histology confirmed calcinosis cutis for scrotal nodule [Figure 2] and benign prostatic hyperplasia for prostatic chips.

- Physical examination findings. Scrotal calcinosis cutis as shown by multiple scrotal nodules, yellow arrow, insert (nodule biopsy specimen, red arrow)
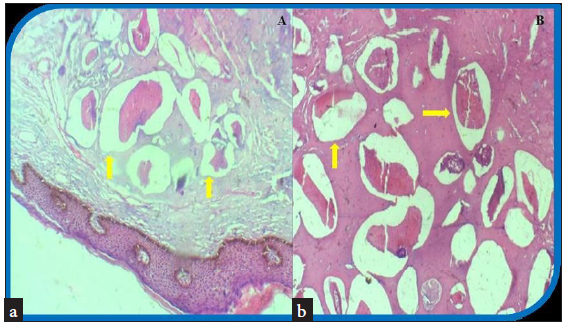
- Histologic findings. (a) Photomicrograph showing keratinized pigmented epidermis overlying calcified masses (yellow arrows) in deep dermal scrotal tissue, no cystic wall or lining (10 x 100 magnifications) (b) Photomicrograph showing calcific subcutaneous masses embedded within fibrocollagenous tissues (yellow arrows) (40 x 100 magnifications).
He did well postoperatively with the resolution of LUTS. However, he declined the excision of scrotal nodules for fear of not wanting open surgical intervention due to its mutilating nature. He was on follow-up observation for two years post-intervention for BPH. He had neither remarkable change in the size and number of the scrotal lesions nor associated distressful symptoms.
DISCUSSION
Idiopathic scrotal calcinosis is a rare and nonmalignant condition. It is caused by an abnormal accumulation of calcium salts in the subcutaneous tissues of the skin and occurs in the absence of metabolic disorders. It was first described in 1883, but the diagnosis was first made by Shapiro et al.[3] in 1970. Scrotal calcinosis cutis commonly affects young Black men aged 20 to 40 years old.[5] Although the index patient is older than 40 years, his black race is consistent with what has been documented in the literature.
As documented in the literature, the index case clinically was seen with firm, multiple, nontender nodules that occupied the whole scrotal area, with sizes varying from a few millimeters to several centimeters. The condition is predominantly asymptomatic but may produce vague pain, itching, discharge, or ulcerations. Our patient had none of these associated symptoms except cosmetic problems, which, according to him and his spouse, are not to be worried about as long as it is a nonmalignant lesions.
Clinically, there is a need to differentiate this condition from other scrotal lesions such as multiple lipodystrophies of the scrotum, angiokeratomas, calcified epithelial tumors, epidermoid cysts, calcified onchocercoma, steatomas, lipoma, fibroma, or even some sexually transmitted diseases that present with subcutaneous nodules on the scrotal skin, such as chlamydial infections or some fungal skin nodules.
Scrotal calcinosis is believed to be idiopathic in most cases though the pathogenesis remains controversial. Dystrophic calcification is secondary to pre existing lesions such as epidermal cysts, eccrine duct milia, or degenerated dartos muscles, which have all been described as possible pathophysiologies.[6] Dubey et al[7] suggested that inflammation of the epidermal cyst resulted in calcification of the cyst wall, which is followed by degeneration of the cyst wall, leaving only the calcific deposits in the older lesions. Dare et al.[8] demonstrated the involvement of eccrine duct milia using immunohistochemistry for CEA antibodies and then proposed the term hydra calcinosis of the scrotal skin. The possible role of nanobacteria in causing extraskeletal calcifications when they invade the skin via the sites of microtrauma without causing overt features of infection was elucidated by Carson.[9] Our index case failed to demonstrate the presence of a cyst wall or keratin around the lesion. This type can be referred to as idiopathic.
The current options of treatment for idiopathic scrotal calcinosis include follow-up observation, medications, cryotherapy or laser, and surgical excision. While nonsurgical options such as drugs and follow-up are ineffective, cryotherapy or lasers are prone to recurrence.[10] Therefore, surgery is the treatment of choice because of the high chances of cure and lower possibility of recurrence. It involves the excision of the diseased tissue intact and reconstruction to close the skin defect.
Despite this, it remains unclear why patients will be reluctant to accept treatment. Some of the reasons for the rejection of surgery include fear of future sexual dysfunction, impaired quality of life, reduced self-esteem, cultural beliefs, and the development of complications. Akinboro et al[4] in a case series reported that two of the three patients declined surgery on account of fear of future reproductive performance. Our index case rejected surgery despite adequate counseling due to fear of mutilation of genital organs, although he consented to bi-TURP, a less invasive endoscopic BPH treatment, as opposed to the invasive open prostatectomy. In addition, with the recent global explosion on the use of information and computer technology, our index patient who was well educated had explored significant information available online about scrotal calcinosis cutis. He already had information about it being a nonmalignant condition and associated risks. Hence, it was not difficult to make his position clear during counseling for intervention.
CONCLUSION
Idiopathic scrotal calcinosis is a rare reactive condition caused by an abnormal accumulation of calcium salts in the subcutaneous tissues of the skin and occurs in the absence of metabolic disorders. It manifests with longstanding nodular skin lesions involving any part of the body, including scrotal skin. Several treatment options are available and should be individualized based mainly on patient preference and availability of treatment modalities, among other considerations. Notwithstanding, it must be clear to the patient that surgery, though invasive, is associated with the least chance of recurrence. Hence, proper patient counseling is paramount to avoid potential medical litigation. Given the available body of evidence on calcinosis cutis, we recommend that patients who declined surgery should be counseled for follow-up and report associated distressful complaints when they supervene.
Acknowledgment
We sincerely appreciate and thank the staff of our health institutions who supported the management.
Ethical approval
The research/study is approved by the Institutional Review Board at Health Research and Ethics Committee (HREC), number UDUTH/HREC/2024/1349, dated 03-01-2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Calcinosis Cutis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
- [Google Scholar]
- Lymphangiomas of the skin with calcified contents. Archives for pathological anatomy and physiology and for clinical medicine. 1883;91:371-3.
- [Google Scholar]
- Idiopathic scrotal calcinosis: report of 2 cases, and review of pathogenesis and factors that determine patients’ acceptance of surgical treatment. Clin Cosmet Investig Dermatol. 2018;11:333-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Case of extensive scrotal calcinosis associated with vitiligo. BMJ Case Rep. 2020;13:e238695.
- [CrossRef] [PubMed] [Google Scholar]
- Scrotal calcinosis: origin from dystrophic calcification of eccrine duct milia. J Cutan Pathol. 1988;15:142-9.
- [CrossRef] [PubMed] [Google Scholar]
- An infectious origin of extraskeletal calcification. Proc Natl Acad Sci U S A. 1998;95:7846-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Systemic sclerosis and calcinosis cutis: response to rituximab. J Clin Pharm Ther. 2016;41:94-6.
- [CrossRef] [PubMed] [Google Scholar]







