Translate this page into:
Prescribing Indicators: A Review in the General Outpatient Clinic of a Nigerian Tertiary Hospital
*Email: ifychijiokenwauche@gmail.com
Abstract
Background:
Evaluating prescription pattern is a measure of drug utilisation review to assess irrational or inappropriate drug use which remains a problem in health facilities. It involves assessing the prescribing, dispensing and distribution of medicines. Studies have shown that more than 50% of all medicines worldwide are incorrectly prescribed. Increased resistance of micro-organisms to antibiotics, drug-drug interaction due to poly-pharmacy are all attributable to inappropriate prescription.
Objective:
The purpose of the study was to evaluate the drug prescription pattern in the General Outpatient Department of a tertiary hospital in Port Harcourt, South-South Nigeria based on WHO prescribing indicators.
Methods:
A cross-sectional retrospective study was carried in the GOPD of the hospital. A total of 2000 prescriptions issued between January to December 2015 were systematically selected and reviewed using the WHO/INRUD prescribing indicators. Data collected were entered into Excel, 2013 and transferred to and analysed with SPSS Version 23 software.
Results:
Out of a total of 6797 drugs prescribed, the average number of drugs prescribed per encounter (ANDPE) was 3.4±1.5, 2411 (35.5%) drugs were prescribed by generic name while 4382 (64.5%) were drugs prescribed by brand names, 4163 (61.3%) drugs were prescribed from the Essential Drug List (EDL) of Nigeria. Observation from the collected data showed that 653 (32.7%) of the total prescriptions analysed contained one or more antibiotics while 29 (1.5%) had one or more injections.Other drugs prescribed include 416 (20.8%) antimalarials, 580 (29%) antipyretics and 475 (23.8%) antihypertensives.
Conclusion:
The study revealed poor compliance to the WHO core prescribing indicators: polypharmacy, poor antibiotics and injection use as well as lack of compliance to EDL prescriptions. There is need for adequate monitoring of prescription writing in the health facility in order to ensure rational drug use.
Keywords
Prescribing Indicators
Rational Drug Use
WHO/INRUD
Introduction
Drug Utilization Review (DUR) has been defined as a structured on-going review of healthcare provider prescribing, pharmacist dispensing, and patient use of medications1. It is a comprehensive, multi-faceted review of patients’ prescription and medication data before, during, and after dispensing to ensure appropriate medication decision making and positive patient outcomes. DUR programmes play a key role in helping managed health care systems understand, interpret, evaluate and improve the prescribing, administration and use of medicines with the primary aim of ensuring rational use of medicines in a population.
Delivery of healthcare to patients involves issuing and dispensing of prescriptions which play a major role in addressing the healthcare needs of patients. According to WHO, a prescription should contain name, age, address of patient, date, strength, dosage form, instructions for use as well as the signature or initials of the prescriber is required and should be tailor-made for an individual patient2,3. Evaluating prescription pattern is a measure of drug utilisation review for rational or inappropriate drug use in health facilities and involves the assessment of prescribing, dispensing and distribution of medicines. According to the WHO, rational drug use implies that patients receive medications appropriate to their clinical needs, in doses that meet their own individual requirements, for an adequate period of time, and at the lowest cost to them and their community4. Appropriate use of drugs is one essential element in achieving quality of health and medical care for patients and the community as a whole.
Using drugs in a way that is non-compliant to the above-definition is termed irrational or non-rational use of drugs and it involves the indiscriminate prescribing of drugs, sometimes in an attempt to satisfy the patient or due to lack of proper clinical knowledge of diagnosis and prescription5. Irrational drug use has also been implicated in the increased rate of morbidity and mortality in infections and chronic diseases such as hypertension, diabetes, epilepsy and mental disorders particularly in children. Other important issues associated with irrational drug use are adverse drug reactions, development of antibiotic resistance as a result of over use, waste of resources and elevated personal expenses.4,6,7
The seriousness of irrational use of medicines can be buttressed by reports indicating the incorrect prescriptions of over 50% of medicines globally, 10-20% of national health budgets of developed countries in comparison to the 20-40 % spent in developing countries, this is in addition to the failure of about 50% patients to use the prescribed medicines4,7–9. Irrational use of medicines is characterized by poly-pharmacy, inadequate dosage of antibiotics, use of antibiotics for non-bacterial infections, low prescribing of generic drugs, low prescribing of drugs on the national Essential Drug List (EDL), using injections in situations when oral medications is more appropriate and generally prescribing inappropriately according to guidelines4,7. The implication of this is that the efforts of drug supply systems as well as the quality health care provided with the very low resources through the countries’ health care sector is undermined10.
To address these issues, drug use indicators for assessing rational use of drugs in health facilities were therefore developed by the World Health Organisation (WHO) together with the International Network for the Rational Use of Drugs (INRUD)11. These include Prescribing, Patient care and Facility indicators. Therefore, this study is aimed at determining prescribing indicators in the health facility by assessment of the of health care providers in terms of average number of drugs prescribed for each patient encounter, percentage of generic drugs prescribed as well as the number of antibiotics prescribed, percentage of encounters with an injection and how much of the drugs were prescribed from the Essential Drugs List or formulary (EDL).
Methods
Study Setting and Design
The present study was conducted at General Out Patient Department (GOPD) of the University of Port Harcourt Teaching Hospital (UPTH), Port Harcourt, Nigeria. Port Harcourt is the capital city of Rivers State. The hospital has 30 departments with an inpatient capacity of about 800 beds. A retrospective cross sectional study was carried out for a duration of five months from September, 2016 to January, 2017. According to WHO standard, 2000 prescriptions from January to December 2015 were sorted into their respective months and days of issue.
Data Collection and Analysis
With the aid of a data collection sheet every third prescription was selected from the bundle of prescriptions issued for any given day such that a minimum of 5 or 150 prescriptions from any given day or month respectively was systematically included in the study sample. Data entered into the data collection sheet include sex, age and prescribing indicators such as name of drug, whether it was brand or generic, number of drugs per encounter, dosage form, therapeutic class, number of drugs prescribed from Essential Drug List (EDL), number of injections, antimalarial prescribed, antipyretic prescribed, number of antibiotics prescribed and number of antihypertensive prescribed. The collected data were analysed based on the WHO prescribing indicators11. The collected data were cross checked for accuracy and entered into Statistical Package for Social Sciences (SPSS) version 23 for descriptive analysis. Frequencies and percentages were calculated and results were presented in form of tables and figures.
Ethical Consideration
The study was approved by the Research Ethics Committee of the University of Port Harcourt Teaching Hospital, Alakahia, Port Harcourt prior to the commencement of the study. (Approval number: UPTH/ADM/90/S.11/ VOL. XI/77; 10th August, 2016). The study was limited to one centre and may not be applicable to other health facilities. Notwithstanding this, the study has provided a template for close monitoring of prescriptions to ensure rationale use of drugs in this facility.
Results
Out of 2000 prescriptions studied a total of 676 (33.8%) had the age of the patient written while 1,324 (66.2%) did not indicate the age. About 68% (1,357) prescriptions (with 515 male and 842 female) had the sex of the patient written while 643 (32.1%) prescriptions had a missing sex. A total of 6,797 drugs were prescribed in the 2,000 prescriptions giving an average of 3.4±1.5 medicines per encounter (Table 1).
| Prescribing indicator | Total drugs/encounters | Average (SD)/percentage | Standard |
|---|---|---|---|
| Drugs per encounter | 6797 | 3.4 (1.5) | 1.6 – 1.8 |
| Drugs prescribed by generic name | 2411 | 35.5% | 100% |
| Drugs prescribed by brand name | 4382 | 64.5% | 0% |
| Drugs from EDL | 4163 | 61.3% | 100% |
| Encounter with antibiotics | 653 | 32.7% | 20.0 – 26.8% |
| Encounters with injection | 27 | 1.4% | 13.4 – 24.1% |
| Encounters with antimalarials | 416 | 20.8% | |
| Encounters with antipyretics | 580 | 29.0% | |
| Encounters with antihypertensives | 475 | 23.8% |
A closer observation of the results reveals that 1352 (67.6%) of the patients had 2-4 drugs prescribed for them while 451 (22.3%) patients had five drugs or more, two patients had 9 prescribed drugs (Figure 1).

- Number of drugs prescribed
From the results obtained, there were 2411drugs prescribed by generic names accounting for 35.5% while the rest were branded (4382; 64.5%). Number of drugs from EDL was 4163 (61.3%), injections (29: 1.5%); while 653 (32.7%) of the analysed prescriptions contained antibiotic drugs. Other drugs prescribed include antimalarials 416 (20.8%), antipyretics 580 (29%) and antihypertensives 475 (23.8%) as shown in Figure 2. More than half (57.7%) of the prescriptions had at least two antihypertensive drugs but the highest number of antihypertensive encounter was 5.
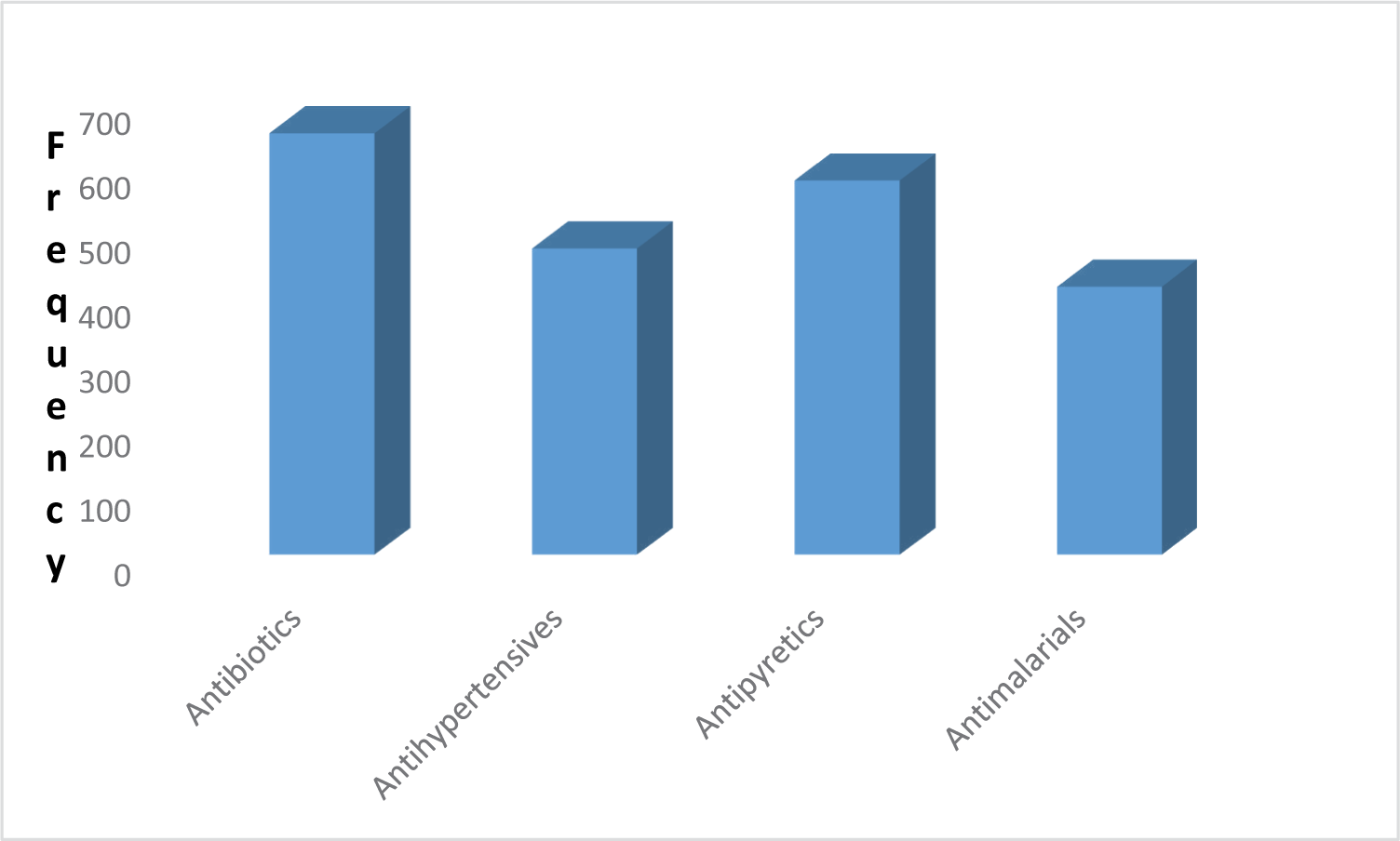
- Classes of drugs prescribed.
Discussion
Rational drug use begins with appropriate prescription which is specific to the individual patient taking into account age, sex, weight, drug and food interactions in addition to the right diagnosis (3). The study reveals that 67.8% prescriptions encountered had a missing age while 32.2% had a missing sex. Therefore, the present study falls short of the above requirement and may impact negatively to the appropriate dispensing of the drug by the pharmacist in ensuring pharmaceutical care to the patient.
The results of 3.4 ±1.5 average number of drugs obtained per prescription and the 9 drugs for a particular encounter is indicative of polypharmacy and falls short of WHO recommended standard of 1.6 to 1.812. This value is in consonance with results obtained from previous studies in Nigeria with reports of 3.4-3.99 but was at variance with studies done in Zimbabwe and Ethiopia where the average obtained was 1.3 and 1.9 respectively8,13–16. The problem of polypharmacy seems to be a common trend among Nigerian prescribers as observed from the previous studies cited. The therapeutic implication of polypharmacy includes increased drug-drug interactions, poor patient adherence, and increased cost of treatment and therefore underlines the need for regular educating of the prescribers.
Generic prescribing of 35.3% obtained in the study is very low in comparison to the 100% recommended standard11. It is equally lower than figures 63%, 82% and 94% obtained from Sudan, Tanzania and Zimbabwe respectively13,16,17. Poor generic prescribing could be attributable to patients’ demand for brand names which they perceive as more effective, pressure from pharmaceutical companies who sometimes offer incentives to the prescribers and inappropriate promotion of medicines11. The fear of fake products cannot be ruled out as part of influence especially in developing countries where the challenge of fake drugs is enormous. Generic prescribing has been shown to put less financial burden in terms of cost of drugs both to the patients and the health establishments as well as reduce the incidence of therapeutic duplication errors10,18,19.
The prescription from EDL from the present study was about half (56.3%) the optimal value of 100% advocated by WHO. Higher values (88%-96%) have been reported from Ethiopia and Tanzania and even higher values from primary health facilities in Nigeria14–17,20. Prescription from EDL makes the procurement, storage and distribution of medicines easier and it is easier to remember fewer items for prescription and dispensing by professionals11.
In our study 1.4% of patients had encounter with injection, a figure much lower than the standard (13.4%-24.1%). This could be attributable to the fact that the study was conducted in the General Outpatients Department which attends only to ambulatory patients, higher figures may be obtained in a cohort of inpatients.
The antibiotics encounter of 38.5 % obtained varies greatly from the WHO reference value of 20.0–26.8 % but lower than values of 45-67.7 % from private and 55-75 % obtained from public facilities in Nigeria21,18,8. There is abounding evidence that overuse of antibiotics potentially leads to antibiotic resistance10,22.
Apart from the spread of resistance, studies have established an association between antibiotics overuse and increase in the risk of adverse reactions, increase in length of disease, increased healthcare costs, increase in mortality and increase in medicalisation of infections that are self-limiting22,23. Other influencing factors include the habit of prescribing by physicians without laboratory investigation and also pressure from patients.
Analysis of other classes of drugs revealed antimalarials to be the least prescribed (20.8%). This is not surprising since many adults in malaria endemic regions are usually asymptomatic- carriers and therefore do not present with clinical malaria. Another important reason may be that many people take antimalarials at home once they have one symptom or another and will not present at healthcare facilities unless there are complications24 The other class of drugs prescribed is antipyretics/ analgesics with a percentage of 29% of which the commonest prescribed drug is paracetamol. This is in consonance with results from an earlier study in Ibadan Southwest Nigeria25. Antipyretic use particularly paracetamol is very common in Nigeria.
Antihypertensive prescriptions accounted for 21.8% of all prescriptions lower than the 30.6% obtained in a rural hospital in western Nigeria. The lower value could be because this was a general clinic for all outpatients unlike the western study which was among the elderly10. Closer observation from the results show that in more than half (57.7%) of the prescriptions there were at least two antihypertensive medications and there were about five in a particular prescription. The prescription of five drugs could be because of comorbidity and possibly severe hypertension which preferably should be referred to a specialist clinic for better management.
Conclusion
The study reveals that only one aspect of the WHO prescribers’ indicators (injection use) was found to fall within the recommended standard. Polypharmacy, brand prescribing, over-prescribing of antibiotics, failure to prescribe from the Essential Drug List were the major criteria that were not met by the health facility. These results underline the need for awareness and makes continuous training of prescribers on the hazards of irrational drug use very imperative in the study area. The establishment of drug and therapeutic committees in health facilities with the mandate of ensuring safe and effective use of medicines would be of help in ensuring rational drug use.
Acknowledgment
We acknowledge the help and support of the Pharmacy staff of the GOPD Unit of the Teaching Hospital for their assistance.
References
- The Academy of Managed Care Pharmacy’s Concepts in Managed Care Pharmacy. 2013. Available from: http://www.amcp.org/ConceptsInManagedCarePharmacy/
- [Google Scholar]
- Guide to good prescribing: a practical manual: Action Programme on Essential Drugs. 1994. WHO. Available from: http://apps.who.int/medicinedocs/pdf/whozip23e/whozip23e.pdf Accessed 25/06/2017
- [Google Scholar]
- Rational drug use in Pakistan: A systematic review. J Pharm Pract Community Med. 2016;24:116-22.
- [CrossRef] [Google Scholar]
- Promoting rational use of medicine: core components. 2002. Available from: http://apps.who.int/medicinedocs/en/d/Jh3011e/
- [Google Scholar]
- Chapter 2, Rational Drug Use. Health Administrator. 2006;19(1):5-7. Available from: http://medind.nic.in/haa/t06/i1/haat07i1p5.pdf
- [Google Scholar]
- WHO medicines strategy 2004-2007 Countries at the core. 2004. WHO/EDM.2004.2. Geneva: World Health Organization; Available from: http://www.who.int/
- [Google Scholar]
- WHO/INRUD drug use indicators at primary healthcare centers in Alexandria, Egypt. Journal of Taibah University Medical Sciences. 2014;9(1):54-64.
- [CrossRef] [Google Scholar]
- Prescribing practices in two health care facilities in warri, Southern Nigeria: A comparative study. Trop J Pharm Res. 2003;2(1):175-82.
- [CrossRef] [Google Scholar]
- Rational use of medicine. International Journal of Pharmaceutical Research. 2010;2:69.
- [Google Scholar]
- Drug prescription pattern in a Nigerian tertiary hospital. Trop J Pharm Res. 2012;11(1):146-52.
- [CrossRef] [Google Scholar]
- How to investigate drug use in health facilities: Selected drug use indicators- EDM research series No. 007. 1993. Available from: http://apps.who.int/medicinedocs/en/d/Js2289e/3.1.html
- [Google Scholar]
- Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5(4):345-51.
- [CrossRef] [PubMed] [Google Scholar]
- INRUD News 1992; 3(1) 9-10. In: In how to investigate drug use in health facilities. Geneva: WHO; 1993. p. :74. (WHO/DAP/93.1)
- [Google Scholar]
- Evaluation of drug use pattern in Lulu Brigg’s Health Centre, University of Port Harcourt, Nigeria using WHO, prescribing indicators. The Pharma Innovation Journal. 2017;6(9):506-510.
- [Google Scholar]
- Assessment of drug use pattern using WHO prescribing indicators at Hawassa University teaching and referral hospital, south Ethiopia: A cross-sectional study. BMC Health Services Research. 2013;13:170.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the Nile province essential drug project, WHO Geneva 1991. WHO/DAP/91.10. In: How to investigate drug use in health facilities. Geneva: WHO; 1993. p. :74. (WHO/DAP/93.1)
- [Google Scholar]
- INRUD News; 3(1) 9. In: In How to investigate drug use in health facilities. WHO: Geneva; 1993. p. :74. (WHO/DAP/93.1)
- [Google Scholar]
- Drug use pattern in out-patient children: A comparison between primary and secondary health care facilities in Northern Nigeria. African Journal of Pharmacy and Pharmacology. 2015;9(4):74-81.
- [CrossRef] [Google Scholar]
- Incidence of adverse drug reactions in hospitalized patients: A meta-analysis of prospective studies. JAMA. 1998;279(15):1200-05.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of prescription pattern and patients’ opinion on healthcare practices in selected primary healthcare facilities in Ibadan, South-Western Nigeria. African Health Sciences. 2015;15(4)
- [CrossRef] [PubMed] [Google Scholar]
- Prescription pattern at a secondary health care facility in Ilorin, Nigeria. Annals of African Medicine. 2007;6(4):186-9.
- [CrossRef] [Google Scholar]
- Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf. 2014;5(6):229-41.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and tolerability of commonly prescribed oral antibiotics for the treatment of respiratory tract infections. Am J Med. 2010;123(4 Suppl):S26-38.
- [CrossRef] [PubMed] [Google Scholar]
- Survey for asymptomatic malaria cases in low transmission settings of Iran under elimination programme. Malar J. 2012;11:126.
- [CrossRef] [PubMed] [Google Scholar]
- Prescriptions involving analgesic drugs at a secondary health facility in Ibadan, Nigeria. Ann Ib Postgrad Med. 2008;6(2):34-8.
- [PubMed] [Google Scholar]






