Translate this page into:
Practice of Breast Self-Examination among Female Students of Chukwuemeka Odumegwu Ojukwu University, Awka
*Email: chymezo@yahoo.com
How to cite this article: Madubogwu CI, Madubogwu NU, Azuike EC. Practice of Breast Self-Examination among Female Students of Chukwuemeka Odumegwu Ojukwu University, Awka. J Health Sci Res 2021;6(2):10-18.
Abstract
Background:
Breast self-examination (BSE) is a reasonably reliable procedure for early detection of breast cancer, especially in limited-resource countries where access to and availability of mammography is inadequate. BSE helps women become familiar with their breasts and increases awareness of breast cancer and breast cancer screening modalities such as clinical breast examination (CBE) and mammography. This study aims at testing the knowledge base of our female university students on breast cancer in addition to the knowledge, attitude, and practice (KAP) of BSE.
Methods:
A cross-sectional descriptive study based on a self-administered pre-tested questionnaire on the KAP of BSE among 284 females students of Chukwuemeka Odumegwu Ojukwu University, Awka. This study was carried out over 3-month period. Data were analyzed with the Spearman’s rank correlation coefficient and Chi-square (χ2) using the IBM Statistical Package for the Social Sciences version 21.
Results:
The mean participants’ age was 20.8 ± 3.3 years. 98.6% have heard of breast cancer, with media and books being the most familiar source of information. Only 60.0% of the participants had been taught BSE, with the most common source of teaching being teachers and parents. 158 (55.6%) of the participants practiced BSE, with only 8.1% ever discovered abnormality. There was a significant association between BSE practice and being taught BSE or hearing about BSE (P < 0.001).
Conclusion:
The knowledge of BSE among the study participants was acquired mainly through books and media though very high, but the level of practice is still shallow. There is a significant association between knowledge and teaching of BSE with the practice of BSE.
Keywords
Breast Self-examination
Knowledge
Practice
University Students
Introduction
A wide range of anomalies (diseases) can affect the breast ranging from benign to malignant varieties. Benign breast diseases are more common than malignant ones.1,2 Breast cancer mortality in the western world is reducing due to early detection and better management resulting from better resources, improved education and increased use of screening mammography.3-5 On the other hand, locally advanced and metastatic breast cancer with attendant morbidity and mortality have remained a significant challenge in developing countries mainly due to ignorance, cultural beliefs, poor or absent cancer registries, lack of proper management protocol, and lack of adequate management protocol inefficient health-care systems.3,6
The first study suggesting the possible effectiveness of breast self-examination (BSE) was published in 1978.7 This study and many additional studies in the premammography era found that women who reported that they perform BSE had their breast cancers detected at a smaller size and at earlier clinical and/or pathologic stage.7 The goal of periodic BSE, as with clinical breast examination (CBE), is to detect palpable tumors. An additional role of BSE is usually to increase awareness of normal breast composition and texture so that there is increased awareness of changes that may be detected during BSE or at some other time.7 There is no evidence that regular performance of BSE will usually lead to detection of breast cancer during a formal BSE procedure.7 Even regular BSE performers commonly detected their breast cancer incidentally, suggesting there is a component of increased body awareness, including its symptoms, in self-performed physical examination.7
Some studies have been done on knowledge, attitude, and practice of BSE among women of various ethnic groups, ages, and social classes with varied results.8-13 In a cross-sectional study of community-dwelling women in Nigeria, women were found to have insufficient knowledge of breast cancer and minority practice BSE and CBE.8 Education appears to be the significant determinant of the level of knowledge and health behavior among their study participants. In a study on market women in Ibadan, Oyo state Nigeria, the level of knowledge and practice of BSE among female traders in Nigeria was unacceptably low and that awareness of BSE was related to educational attainment.9 Another study among female health workers in a teaching hospital in Sagamu, Nigeria found out that medical doctors had more knowledge about breast cancer than nurses and laboratory scientists.11 The study also indicated that nurses have a poor attitude toward BSE, which affects their practice. They recommended that BSE be included in both undergraduate and postgraduate courses, especially for nurses, as they are primarily involved in patient education. A similar study was done in Benin city, Nigeria, among female health workers, noted that though female health workers are expected to act as role models and help in educating the public, they had insufficient knowledge of the risk factor for breast cancer and practice of breast cancer screening.12 Furthermore, in another study among female undergraduates in Kwara state, Nigeria, it was noted that although the majority of respondents were aware of breast cancer as a disease entity, their knowledge and understanding of the disease were meager.10
BSE has many benefits: easy to learn, cost-effective to the patient, high patient acceptability, and noninvasive procedure.14-17 Other advantages are that it is a reasonably reliable procedure for early detection of breast cancer, it helps women to be familiar with their breasts and increases awareness of breast cancer and other breast cancer screening modalities such as CBE and mammography.14-17 BSE also has some shortcomings like: it requires a lot of patient motivation for regular practice, can only detect palpable breast lesions, it increases benign breast biopsy rate, and there is difficulty in measuring adherence and competence.7
In low and medium-income countries, BSE is still very relevant as a means of cancer detection because up to 90% of the breast cancers in these regions are still self- detected.15,18 Despite the stated benefits of BSE, previous studies on knowledge of breast cancer as well as knowledge, attitude, and practice (KAP) of BSE across various strata of women in the region have shown varied results.8-13 The current study aims to test the knowledge base of female students of the Chukwuemeka Odumegwu Ojukwu University, Awka, on breast cancer and the knowledge, attitude, and practice of BSE. This study is relevant because educated women are role models of healthy and modern society.
Materials and Methods
This is a cross-sectional descriptive study on the KAP of BSE among females of a tertiary institution in Anambra state. The study was based on the self-administered pre-tested questionnaire. The questionnaire consists of 30 close-ended questions on KAP tailored for BSE as well as knowledge on breast cancer. Ethical approval was sort and gotten from the Institutional ethical committee with Health Research Committee assigned number: COOUTH/ CMAC/ETH.C/VOL.1/FN:04/0071. A written informed consent was obtained from each one of the participating students before enrolling into the study. The students refusing to consent were excluded from the study. The information sort through the questionnaire includes questions on social demographic data, knowledge, attitude, and BSE and breast cancer practice.
We analyzed the data with the aid of the IBM Statistical Package for the Social Sciences version 21, and the results were presented in the chart, frequency tables, and percentages. The correlation was done using Spearman’s rank correlation coefficient and chi-square (χ2). According to statistical analyses, P < 0.05 is considered statistically significant.
Results
A total number of 284 participants took part in the study and were used for the analytical part of the study, and the mean age of the participants was 20.8 years, with a standard deviation of 3.3 years. The majority of the participants were from Anambra State and single marital status (Table 1). In addition, 136 (47.9%) of the participants were from the Pharmacy department and 87 (30.7%) from the Medicine Department (Figure 1).
| Variables | Frequency (n=284) | Percentage |
|---|---|---|
| Age (mean±standard deviation) in years | 20.8±3.3 | |
| Level | ||
| 100 | 21 | 7.4 |
| 200 | 77 | 27.1 |
| 300 | 73 | 25.7 |
| 400 | 50 | 17.6 |
| 500 | 42 | 14.8 |
| 600 | 21 | 7.4 |
| State of origin | ||
| Abia | 5 | 1.8 |
| Anambra | 243 | 85.9 |
| Delta | 7 | 2.5 |
| Ebonyi | 2 | 0.7 |
| Edo | 1 | 0.4 |
| Enugu | 2 | 0.7 |
| Imo | 23 | 8.1 |
| Marital status | ||
| Married | 14 | 5.0 |
| Single | 268 | 95.0 |
Table 1 revealed that the mean age of the participants was 20.8 years with a standard deviation of 3.3 years. The majority of the participants were from Anambra State and single marital status
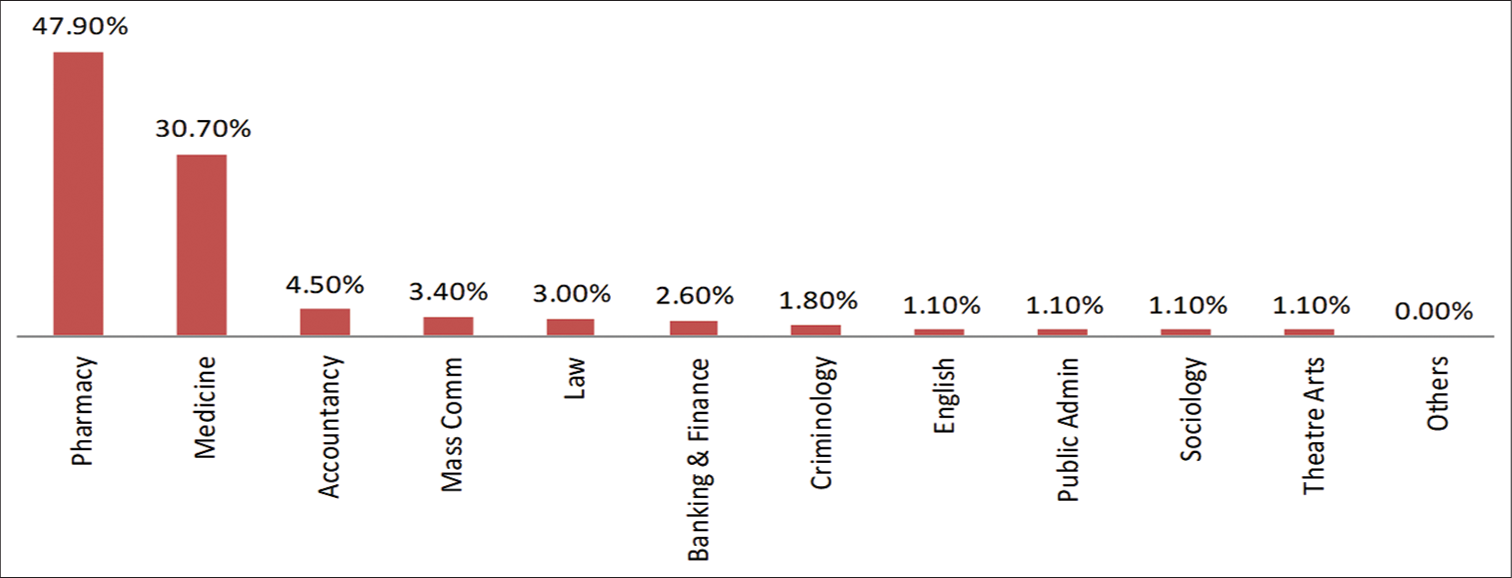
- Department of participants.
247 (87.0%) of the participants have heard of BSE, with the most typical source of information being media and books (Table 2). Almost all the participants (98.6%) have heard of breast cancer, with media and books being the most familiar source of information. More than half of the cases (56.3%) with a positive history of breast cancer had aunts mostly affected (Table 3). 242 (85.2%) of the participants appreciate BSE to be helpful for the detection of breast cancer. However, only 60.0% of the participants had been taught BSE, with the most common source of teaching being teachers and parents (Table 4). 195 (68.7%) of the participants agree that BSE should begin before puberty but had no idea when best to do it (60.2%) (Table 5). 232 (82.0%) of the participants agree that BSE should be done by each individual person, using the hand in 237 (88.8%), and by feeling the breast with the hand in 190 (66.9%) (Table 6).
| Variables | Frequency (N = 284) | Percentage |
|---|---|---|
| Have you heard of BSE? | ||
| No | 37 | 13.0 |
| Yes | 247 | 87.0 |
| Source of information (BSE) | ||
| Books | 70 | 28.6 |
| Media | 110 | 44.9 |
| Hospital | 13 | 5.3 |
| Conferences/seminar | 22 | 9.0 |
| Lecture | 14 | 5.7 |
| Friends | 10 | 4.1 |
| Missing values | 6 | 2.4 |
BSE: Breast self-examination. 247 (87.0%) of the participants have heard of BSE, with the most typical source of information being media and books (Table 2)
| Variables | Frequency (n=284) | Percentage |
|---|---|---|
| Have you heard of breast cancer? | ||
| No | 3 | 1.1 |
| Yes | 280 | 98.6 |
| Missing values | 1 | 0.4 |
| Source of information (Breast Cancer) | ||
| Books | 100 | 35.8 |
| Media | 111 | 39.8 |
| Hospital | 12 | 4.3 |
| Conferences/seminar | 23 | 8.2 |
| Lecture | 23 | 8.2 |
| Friends | 4 | 1.4 |
| Missing value | 6 | 2.2 |
| Any family history of breast cancer | ||
| No | 256 | 90.1 |
| Yes | 20 | 7.1 |
| Missing values | 8 | 2.8 |
| Relationship with breast cancer patient | ||
| Mother | 3 | 18.7 |
| Aunt | 9 | 56.3 |
| Grandmother | 4 | 25.0 |
Table 3 shows that almost all the participants (98.6%) have heard of breast cancer, with media and books being the most typical source of information. In addition, more than 50% of the participants (56.3%) with a positive history of breast cancer had aunts mostly affected
| Variables | Frequency (n=284) | Percentage |
|---|---|---|
| Awareness of BSE as useful tool for the detection of breast cancer | ||
| No | 36 | 12.7 |
| Yes | 242 | 85.2 |
| Missing values | 6 | 2.1 |
| Have you been taught BSE? | ||
| No | 105 | 37.0 |
| Yes | 171 | 60.2 |
| Missing values | 8 | 2.8 |
| Who taught you BSE? | ||
| My parents | 39 | 27.9 |
| Teacher | 44 | 31.1 |
| Doctor | 31 | 22.1 |
| Nurse | 5 | 3.6 |
| Friend | 21 | 15.0 |
A good proportion of the participants appreciates BSE to be helpful for the detection of breast cancer. Only 60.0% of the participants had been taught BSE, with the most typical source of teaching being teachers and parents (Table 4)
| Variables | Frequency (n=284) | Percentage |
|---|---|---|
| When to begin BSE? | ||
| From puberty | 195 | 68.7 |
| From 20 years | 22 | 7.7 |
| From 30 years | 1 | 0.4 |
| After menopause | 1 | 0.4 |
| No idea | 58 | 20.4 |
| Missing value | 7 | 2.5 |
| BSE is usually done? | ||
| Daily | 32 | 11.3 |
| Weekly | 36 | 12.7 |
| Monthly | 104 | 36.6 |
| Yearly | 8 | 2.8 |
| No idea | 97 | 34.5 |
| Missing value | 7 | 2.5 |
| BSE is best done? | ||
| During menstrual flow | 14 | 4.9 |
| A week after period | 86 | 30.3 |
| During pregnancy | 1 | 0.4 |
| During breastfeeding | 2 | 0.7 |
| No idea | 171 | 60.2 |
| Missing values | 10 | 3.5 |
Table 5 shows that the majority of the participants (68.7%) agree that BSE should begin before puberty but had no idea when best to do it (60.2%)
| Variables | Frequency (n=284) | Percentage |
|---|---|---|
| BSE is to be done by? | ||
| Doctor | 35 | 12.1 |
| Trained Nurse | 9 | 3.3 |
| The Individual | 232 | 82.0 |
| Missing values | 8 | 2.8 |
| BSE is usually done with? | ||
| Ultrasound | 6 | 2.2 |
| Mammography | 10 | 3.7 |
| Hand | 237 | 88.8 |
| Missing values | 14 | 5.2 |
| BSE is done by? | ||
| Inspecting the breast in the mirror | 53 | 18.7 |
| Feeling the breast with the hand | 190 | 66.9 |
| Feeling the armpit with the hand | 10 | 3.5 |
| Doing ultrasound of the breast | 6 | 2.1 |
| Mammography | 2 | 0.7 |
| Missing values | 23 | 8.1 |
Table 6 revealed that most of the participants agree that BSE should be done by each individual person (82.0%), with the hand (88.8%), and by feeling the breast with the hand (66.9%)
Early detection of breast cancer was observed as the most familiar benefit of BSE by the participants. 172 (61.2) of the participant would want to see the doctor when an abnormality is discovered (Table 7). 158 (55.6%) of the participants practiced BSE, with only 23 (8.1%) ever found the anomaly. Among those that discovered abnormality, 15 (68.5%) saw their doctor (Table 8). There was a significant level of association between the practice of BSE and being taught BSE or hearing about BSE (P < 0.001) (Table 9).
| Variables | Frequency (n=284) | Percentage |
|---|---|---|
| What are the benefits of BSE | ||
| Used in breast USS | 2 | 0.7 |
| Used in mammography | 5 | 1.8 |
| Can aid early detection of breast cancer | 249 | 87.7 |
| Missing value | 28 | 9.9 |
| What to do when abnormality is discovered during BSE | ||
| Pray over it | 12 | 4.3 |
| Do some lab test | 80 | 28.5 |
| See my doctor | 172 | 61.2 |
| Missing values | 17 | 6.0 |
| Do you think BSE is a good practice? | ||
| No | 1 | 0.4 |
| Yes | 265 | 93.3 |
| Missing values | 18 | 6.3 |
| Variables | Frequency (n=284) | Percentage |
|---|---|---|
| Do you practice BSE | ||
| No | 108 | 38.0 |
| Yes | 158 | 55.6 |
| Missing values | 18 | 6.3 |
| Have you ever discovered abnormality since the practice of BSE | ||
| No | 203 | 71.5 |
| Yes | 23 | 8.1 |
| Missing values | 58 | 20.4 |
| Actions taken on seeing abnormality during BSE | ||
| Did some lab tests | 1 | 4.5 |
| Saw my doctor | 15 | 68.5 |
| Did nothing | 3 | 13.6 |
| Missing values | 3 | 13.6 |
Table 8 shows that little above half of the participants (55.6%) practiced BSE, with only 8.1% ever discovered abnormality. Among those that discovered abnormality, the majority (68.5%) saw their doctor
| Variable | Do you practice BSE? | χ2 | P-value | |
|---|---|---|---|---|
| No (%) | Yes (%) | |||
| Marital status | ||||
| Married | 2 (1.9) | 11 (7.0) | 3.547 | 0.081 |
| Single | 105 (98.1) | 147 (93.0) | ||
| Heard of BSE | ||||
| No | 31 (28.7) | 2 (1.3) | 44.897 | <0.001 |
| Yes | 77 (71.3) | 155 (98.1) | ||
| Missing values | 0 (0.0) | 1 (0.6) | ||
| Have you been taught of BSE | ||||
| No | 76 (70.4) | 20 (12.7) | 106.711 | <0.001 |
| Yes | 27 (25.0) | 138 (87.3) | ||
| Missing values | 5 (4.6) | 0 (0.0) | ||
Table 9 revealed that there was a significant association between practice of BSE and being taught BSE or hearing about BSE (P < 0.0)
Early detection of breast cancer was observed as the most familiar benefit of BSE by the participants. Most of the participants (61.2%) would want to see the doctor when an abnormality is discovered.
Discussion
The incidence, mortality, and morbidity of breast cancer in developing countries are rising.3,6,19 This has been attributed to poor awareness of symptoms and risk factors for breast cancer and the low availability of modern breast cancer screening facilities.3,6 BSE though not the ideal tool for detecting breast cancer can be of immense use in areas where mammography facility is still inadequate. BSE, when thought the young girls can create awareness for breast cancer and inculcate good breast care practices early in the lives of our women.
The social demographic data in this study show that the age means for the participants were 20.8 ± 3.3, which is consistent with similar studies involving female tertiary institution students.15,16 The study also showed that most of the students were from Anambra State mainly because the institution is a state-owned university. The majority of the participants were unmarried, probably because of the age range of the study population, which was at the early adult stage (Table 1). 223 (78.6%) of the participants were either studying medicine (47.9%) or pharmacy (30.7%) (Figure 1), probably because their course is medically oriented and understood the importance of the study thereby were willing to cooperate more.
The majority of the participants (87.0%) have heard of BSE, with the most typical source of information being media and books (Table 2). The knowledge level in this study is relatively high because of the literate status of the participants who are University students. This correlates with Nde et al. in Camaroon16, Casimir et al.,20 and Salaudeen et al.10 in Nigeria, all conducted among tertiary students. This high level of knowledge contrast sharply with low levels recorded by other studies done in Nigeria among rural and market women.21-23 Another analysis also done in Nigeria demonstrated that educational level is a significant component of the level of knowledge and health behavior among their study participants.8 The source of information for the majority of the participants in this study was media and books, which agrees with the finding of media as the primary source in another survey in Camaroon.16
Almost all the participants (98.6%) have heard of breast cancer, with media and books being the most typical source of information (Table 3). This correlates with the finding of 97.2% by Salaudeen et al. in their study and that electronic and print media were the primary sources of information.10 Only 7.1% of the participants had a positive family history of breast cancer, with more than half (56.3%) involving the aunts (Table 3). The fact that media and books were the primary sources of information for the study population for both BSE and breast cancer reiterates the need for their use to enhance public health education.
A good proportion of the participants (85.2%) appreciates BSE to be helpful for the detection of breast cancer. Only 60.2% of the participants had been taught BSE, with the most typical source of teaching being teachers and parents (Table 4). This finding that teaching BSE was mainly by teachers and parents is worrisome because the source of information determines the quality of the knowledge. Health workers, particularly the doctors and nurse with their knowledge base, should have been at the fore front, but they are only responsible for 22.1% and 3.6%, respectively (Table 4). The majority of the participants (68.7%) agree that BSE should begin before puberty but had no idea when best to do it (60.2%) (Table 5). In a similar study by Casimir et al., although the awareness of BSE was very high at 98.9%, only 20.5% knew the right age to begin BSE.20 Furthermore, in the study by Faronbi and Abolade among female secondary school teachers in a rural community, only 16.0% of their participants knew when to start BSE.24
Most of the participants agreed that BSE should be done by each individual person (82.0%), with the hand (88.8%), and by feeling the breast with the hand (66.9%) (Table 6). This shows that the level of knowledge by the study population in terms of resources and method of BSE was very high. Aiding early detection of breast cancer was correctly observed as the most familiar benefit of BSE by the participants (87.7%) (Table 7). In a similar study by Nde et al., 88.6% knew that BSE is essential for early detection of breast cancer.16 Furthermore, most participants (61.2%) would want to see the doctor when an abnormality is discovered (Table 7). This finding is encouraging because one of the significant reasons for BSE is finding breast abnormality early and seeking medical care.25-27
158 (55.6%) of the participants practiced BSE, with only 8.1% ever discovering an aberration (Table 8). Among those who discovered abnormality, most (68.5%) saw their doctor (Table 8). The level of practice of BSE in this study is above average and correlates with the finding in other studies also done in Nigeria.28-31 This is in contrast to some other studies also in Nigeria that recorded low levels of practice of BSE: 13.0%; 32.5%; 31.4%; 12.0%; 11.7%; and 0.4% by Makanjuola et al.23; Casimir et al.20; Isara et al.32; Olowokere et al.33; Faronbi et al.24; and Obaji et al.21 respectively. All these studies with the common low practice of BSE records were either done in secondary students or among market women. However, this implies that the level of education has a lot to do with BSE.
In the present study, there was a significant association between BSE practice and being taught BSE or hearing about BSE (P < 0.001). There was, however, no meaningful relationship between marital status and the practice of BSE (Table 9). This shows that the practice of BSE can be enhanced by creating awareness and by also teaching BSE. In a study conducted among female university students in Cameroon, a significant association was observed between knowledge and attitude with the tendency to practice BSE.16 Furthermore, in a survey by Haji-Mahmoodi et al. among health workers in Iran, they found significant associations between the practice of BSE with age, the level of education, personal history of breast problems, and knowledge of how to examine the breasts.34
Conclusion
The knowledge of BSE among the study participant was acquired mainly through books and media though very high, but the level of practice is still shallow. The study established a significant association between knowledge and teaching of BSE with the practice of BSE. Efforts should be geared toward improving the understanding of BSE through education. This will, in turn, impact the practice level, of course.
References
- The breast In: Williams NS, Christopher JK, O'Connell PR, eds. Bailey and Love's Short Practice of Surgery (25th ed). London: Edward Arnold Ltd; 2008. p. :827-48.
- [Google Scholar]
- Changing pattern of benign breast lumps in young females. World J Med Sci. 2007;2:21-4.
- [Google Scholar]
- Temporal trends in breast cancer presentation in the third world. J Exp Clin Cancer Res. 2008;27:17.
- [CrossRef] [PubMed] [Google Scholar]
- Breast fine needle aspiration cytology in a Nigerian tertiary hospital. East Central Afr J Surg. 2007;12:126-32.
- [Google Scholar]
- Locally advanced breast cancer: Treatment guideline implementation with particular attention to low-and middle-income countries. Cancer. 2008;113:2315-54.
- [CrossRef] [PubMed] [Google Scholar]
- The Impact of Neoadjuvant chemotherapy on patients with locally advanced breast cancer in a Nigerian semiurban teaching hospital: A single-center descriptive study. World J Surg. 2010;34:1771-8.
- [CrossRef] [PubMed] [Google Scholar]
- American cancer society guidelines for breast cancer screening update. Cancer J Clin. 2003;53:141-69.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, attitude and practice of Nigerian women toward breast cancer: A cross sectional study. World J Surg Oncol. 2006;4:4-11.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge and practice of BSE among female traders in Ibadan, Nigeria. Ann Ibadan Postgrad Med. 2005;3:52-6.
- [CrossRef] [Google Scholar]
- Knowledge and attitude to breast cancer and BSE among female undergraduates in a state in Nigeria. Eur J Soc Sci. 2009;7:157-65.
- [Google Scholar]
- knowledge, attitude and practice of BSE in female health workers in Olabisi Onabanjo university teaching hospital, Sagamu, Nigeria. Int Med J. 2009;8:1.
- [CrossRef] [Google Scholar]
- knowledge, attitudes and practice of breast cancer screening among female health workers in a Nigerian urban city. BMC Cancer. 2009;9:203.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge and attitudes of BSE in a group of women in Shiraz, Southern Iran. Postgrad Med J. 2009;85:283-7.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, attitude, and practice of breast self-examination amongst female IT professionals in Silicon Valley of India. J Family Med Prim Care. 2019;8:568-72.
- [CrossRef] [PubMed] [Google Scholar]
- Breast self-examination: Knowledge, attitude, and practice among female dental students in Hyderabad city, India. Indian J Palliat Care. 2012;18:68-73.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, attitude and practice of breast self-examination among female undergraduate students in the university of Buea. BMC Res Notes. 2015;8:43.
- [CrossRef] [PubMed] [Google Scholar]
- Women's knowledge, attitude, and practice of breast self-examination in Sub-Saharan Africa: A scoping review. Arch Public Health. 2020;78:84.
- [CrossRef] [PubMed] [Google Scholar]
- Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge and practice of breast self-examination among female undergraduates in SouthEastern Nigeria. Health. 2015;7:1134.
- [CrossRef] [Google Scholar]
- Awareness and practice of breast self. Examination among market women in Abakaliki. South East Nigeria. Ann Med Health Sci Res. 2013;3:7-12.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge and beliefs of breast self-examination and breast cancer among market women in Ibadan, South West, Nigeria. PLoS One. 2015;10:e0140904.
- [CrossRef] [PubMed] [Google Scholar]
- Breast cancer: Knowledge and practice of breast self examination among women in rural community of Ondo. . 2013;8:32-7.
- [CrossRef] [Google Scholar]
- Breast self examination practices among female secondary school Teachers in a rural community in Oyo State, Nigeria. Open J Nurs. 2012;2:111-5.
- [CrossRef] [Google Scholar]
- Improving early detection of breast cancer in sub-Saharan Africa: Why mammography may not be the way forward. Glob Health. 2019;15:3.
- [CrossRef] [PubMed] [Google Scholar]
- Breast self-examination: Defining a cohort still in need. Am J Surg. 2009;198:575-9.
- [CrossRef] [PubMed] [Google Scholar]
- Breast self examination-a necessary preventive tool: Knowledge and practice among students of college of education Gindiri, Plateau state. Jos J Med. 2012;6:47-53.
- [Google Scholar]
- Knowledge and practice of breast self-examination among female undergraduate students. Ann Afr Med. 2009;8:55-8.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge and practice of self-breast examination among female undergraduate students in a Northern Nigeria university. J Med Biomed Res. 2013;12:62-8.
- [Google Scholar]
- Breast self examination practice among female students of tertiary institutions. J Educ Pract. 2016;7:11-8.
- [Google Scholar]
- Breast self-examination as a method of early detection of breast cancer: Knowledge and practice among antenatal clinic attendees in South Eastern Nigeria. Pak J Med Sci. 2009;25:122-5.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge of breast cancer and practice of breast self examination among female senior secondary school students in Abuja, Nigeria. J Prev Med Hyg. 2011;52:186-90.
- [Google Scholar]
- Breast cancer knowledge and screening practices among women in selected rural communities of Nigeria. J Public Health Epidemiol. 2012;4:238-45.
- [CrossRef] [Google Scholar]
- Breast self-examination: Knowledge, attitudes, and practices among female health care workers in Tehran, Iran. The Breast J 2002. ;. ;8:222-5.
- [CrossRef] [PubMed] [Google Scholar]






