Translate this page into:
Occurrence and management of lower respiratory tract infections in children at a Nigerian tertiary hospital
*Corresponding author: Dr. Patricia Uche Ogbo, Department of Clinical Pharmacy & Biopharmacy, Faculty of Pharmacy, University of Lagos, Akoka, Lagos, Nigeria. pogbo@unilag.edu.ng
-
Received: ,
Accepted: ,
How to cite this article: Okonkwo CA, Ogbo PU, Ayeni FA, Akande AA. Occurrence and management of lower respiratory tract infections in children at a Nigerian tertiary hospital. J Health Sci Res. 2024;9:60-5. doi: 10.25259/JHSR_52_2023
Abstract
Objectives
Infectious diseases such as pneumonia, diarrhea, and malaria are the major causes of child mortality, with pneumonia, a lower respiratory tract infection (LRTI), being the foremost of the three. Antimicrobial agents are required to treat LRTIs, such as pneumonia caused by bacteria, while those commonly caused by viruses, such as bronchiolitis, do not benefit from antimicrobial therapy unless laboratory tests indicate otherwise. When not shown, empirical management of patients using antimicrobials remains a risk factor for antimicrobial resistance in the management of LRTIs. This study aimed to determine the occurrence of LRTIs in children who presented with acute respiratory tract infections (RTIs) and evaluate their management in comparison with the guidelines.
Material and Methods
The study was a descriptive retrospective review of prescribing records for respiratory tract infections (RTIs) presented at the Alex Ekwueme Federal University Teaching Hospital, Abakaliki (AE-FUTHA), Ebonyi State, Nigeria. Data were collected through systematic sampling of the case folders of children aged five years and below who presented with RTIs from January to December 2021, using a data collection proforma. Collected data were cleaned and coded, and Statistical Package for Social Sciences (SPSS) Version 28 was used for analysis.
Results
There were 422 case folders containing diagnoses of RTIs. Of these, 36 (8.5%) were diagnosed with LRTIs and 28 (6.6%) had no comorbidity. Of the 28 cases without comorbidities, pneumonia (20;71.4%) and bronchiolitis (8;28.6%) were the only two LRTIs. Antibiotics were the most prescribed medications, followed by vitamins (8;28.6%) and antihistamines (7;25.0%). There were seven types and three combinations of antibiotic medications, the most being cefuroxime (10;35.7%) followed by amoxicillin/clavulanic acid (7; 25.0%). One case of pneumonia did not receive an antibiotic. Laboratory investigations were not conducted for the majority (25;89.3%) of the cases presented.
Conclusion
This study showed that the LRTIs presented were mostly managed using the recommended antibiotics for pneumonia. Antibiotics for bronchiolitis without confirmation by laboratory tests may not have been justified as most of them are of viral origin. Deviations from guidelines may be reduced if national protocols are developed in managing LRTIs.
Keywords
Lower respiratory tract infections
Children
Antibiotics
Pneumonia
INTRODUCTION
According to recent data, pneumonia, a lower respiratory tract infection (LRTI), has remained the leading cause of global death in under-fives, with Sub-Saharan Africa and Asia accounting for about 70% of the reported cases.[1–3] In 2019 alone, pneumonia caused 14% of all deaths in under-fives.[4] In Nigeria, a study conducted in Ilorin found that pneumonia accounted for 13.3% of hospital admissions within the time of the study.[5] Other LRTIs include bronchitis, mainly in adults, and bronchiolitis, which is more prominent in children. Viruses cause bronchitis and bronchiolitis, requiring symptomatic treatment except when laboratory tests indicate otherwise. Pneumonia is majorly caused by bacteria, such as Streptococcus Pneumonae, Mycobacterium pneumonia, Chlamydia spp, Legionella spp, and Coxiella burnetti, with a few of viral origin.[6] Antibiotics are required to treat LRTIs caused by bacteria, specifically pneumonia, and those of viral origin, such as bronchitis and bronchiolitis, can run their course and should not be treated using antibiotics.[7–8] However, it is challenging to distinguish between bacterial and viral LRTIs without testing. This introduces problems of overuse or underuse of antibiotics in the therapy of LRTIs, potentially creating a problem of antimicrobial resistance.[9] Standard treatment guidelines for Nigeria indicate that tests such as sputum examination, hematological evaluation, sputum culture, chest radiogram, blood cultures, and serologic studies should be conducted when suspected pneumonia cases are presented.[10] However, the pediatric association of Nigeria’s treatment guidelines indicated that there is no need for these tests for patients with community-acquired pneumonia and that empirical treatment with recommended antibiotics is safe.[11]
With regard to the treatment of pneumonia, the Nigerian standard treatment guidelines indicate age-appropriate doses of co-amoxiclav, benzylpenicillin (intravenous), and cefuroxime as standard treatments for pneumonia in children. At the same time, the WHO and the pediatric association of Nigeria recommend amoxicillin as the first-line antibiotic.[4,11] Some authors have observed macrolide antibiotics being effective for community-acquired pneumonia patients.[12] Nevertheless, authors have recommended that unless pneumonia is suspected, clinicians should provide safety netting advice for children presenting with chest infections rather than prescribe antibiotics.[13] With growing evidence of antimicrobial resistance, empirical treatment is becoming more challenging and a public health problem.[12] While ensuring that antibiotics are used appropriately, some findings showed that only one-third of children with pneumonia receive the antibiotics they need.[4,6] Meanwhile, children with upper respiratory tract infections received antibiotics mainly inappropriately.[14,15] In Botswana, a study conducted in the primary health centers found that phenoxymethylpenicillin and amoxicillin were the most prescribed for children with pneumonia.[16]
Since studies conducted in tertiary institutions on LRTIs in Nigeria are scarce, this study was designed to determine the occurrence of LRTI among children attending a tertiary hospital and assess its management, comparing it with the WHO, pediatric association of Nigeria, and the Nigerian standard treatment guidelines.
MATERIAL AND METHODS
Study settings
This study was conducted at Alex Ekwueme Federal University Teaching Hospital, Abakaliki (AE-FUTHA), Ebonyi State, Nigeria. The study was conducted in the children’s outpatients clinic of AE-FUTHA.
Study design
The study was a descriptive retrospective review of the presentation of acute RTIs and prescribing records for LRTIs encountered from January 2021 to December 2021 presented in the children’s outpatients’ clinic. The period of 12 months was used to ensure an adequate number of cases for proper assessment.
Study population
The study population included case folders of children aged five years and below diagnosed with RTIs. This was sampled from the records of outpatients who presented and were treated for RTIs within the study period.
Sampling technique and data collection
Systematic sampling of five working days was used to select cases of RTIs that were presented in the children’s outpatient department of the hospital during the study period (January–December 2021). The first five working days of each month were used to accommodate all prescribers because the prescribers consulted on different working days of the week.
Data were collected using an adapted proforma, which had been used in a similar study.[17] Information was extracted from children’s outpatient clinic registers, where all prescribing details were recorded. The variables collected include the date of prescription, gender of the child, age of the child (in months), complaints, diagnoses, investigations done, and medicines prescribed.
Data collected during data analysis were coded and entered into Statistical Package for Social Sciences (SPSS) Version 28.0. Data was cleaned and then analyzed. Results were presented as proportions (percentages) and frequencies using frequency tables and bar chart. A comprehensive guideline for the management of LRTIs as provided by the Nigerian standard treatment guidelines, the World Health Organization, and the pediatric association of Nigeria were used to evaluate the medications prescribed.
Ethical approval
Ethical approval was obtained from the Health Research and Ethics Committee of Alex Ekwueme Federal University Teaching Hospital, Abakaliki (AE-FUTHA/REC/VOL 3/2022/008). Approval to work and access data in the pediatrics department was obtained from the head of the department of the pediatrics unit.
RESULTS
Four hundred and twenty-two cases of respiratory tract infections were collected within the study period. Of these, 386 (91.5%) were upper respiratory tract infections, while 36 (8.5%) were LRTIs. Of the 36 LRTIs, 28 (6.6%) were without comorbidities. This paper is focused on LRTIs without comorbidities.
Gender and age categories
The LRTI cases found were from 12 (42.9%) male and 16 (57.1%) female children. The highest (13; 46.4%) occurrence of LRTI was in the 1–11 age category, followed by the 12–23 age category [Table 1].
| Variable | Characteristics | Frequency (%) (n = 28) |
|---|---|---|
| Gender | Male | 12 (42.9) |
| Female | 16 (57.1) | |
| Age (months) | <1 | 1 (3.6) |
| Mean age = 18.32 ± 18.744 months | 1–11 | 13 (46.4) |
| 12–23 | 5 (17.9) | |
| 24–35 | 3 (10.7) | |
| 36–47 | 2 (7.1) | |
| 48–59 | 2 (7.1) | |
| 60 | 2 (7.1) |
Types of LRTI diagnosis and laboratory tests conducted
There were two types of LRTI diagnosed: pneumonia (20;71.4%) and bronchiolitis (8:28.6%). No laboratory tests were conducted for 18 pneumonia cases and seven bronchiolitis cases. The tests conducted are presented in Table 2.
| Tests | Pneumonia | Bronchiolitis | Total |
|---|---|---|---|
| Nil | 18 (64.2) | 7 (25.0) | 25 (89.2) |
| Full blood count & malaria parasite | 0 (0.0) | 1 (3.6) | 1 (3.6) |
| Full blood count, blood film, & chest X-ray | 1 (3.6) | 0 (0.0) | 1 (3.6) |
| Microscopy culture, sensitivity, & Mantoux | 1 (3.6) | 0 (0.0) | 1 (3.6) |
| Total | 20 (71.4) | 8 (28.6) | 28 (100.0) |
Medications prescribed
Nine drug classes were prescribed for the diagnosed LRTIs, with antibiotics as the most prescribed in 25 (89.3%) out of 28 prescriptions [Figure 1].
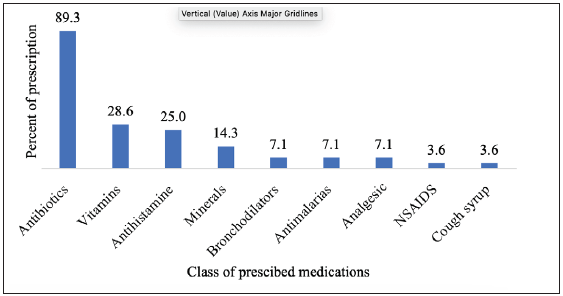
- Class of medications prescribed for diagnosed lower respiratory tract infections.
Antibiotics prescribed for pneumonia and bronchiolitis
The most prescribed antibiotic was cefuroxime (10;35.7%), followed by amoxicillin/clavulanate (7;25.0%). There were four sets of combinations of two different antibiotics [Table 3].
| Antibiotics prescribed |
Pneumonia n (%) |
Bronchiolitis n (%) |
Total n (%) |
|---|---|---|---|
| Nil | 1 (3.6) | 0 (0.0) | 1 (3.6) |
| Amoxicillin/clavulanate | 7 (25) | 0 (0.0) | 7 (25) |
| Cefuroxime | 5 (17.85) | 5 (17.85) | 10 (35.7) |
| Cefuroxime, erythromycin | 0 (0.0) | 2 (7.1) | 2 (7.1) |
| Amoxicillin/clavulanate, Azithromycin | 3 (10.7) | 0 (0.0) | 3 (10.7) |
| Ceftriaxone, gentamycin | 1 (3.6) | 0 (0.0) | 1 (3.6) |
| Cefuroxime, azithromycin | 2 (7.1) | 1 (3.6) | 3 (10.7) |
| Erythromycin | 1 (3.6) | 0 (0.0) | 1 (3.6) |
| Total | 20 (71.45) | 8 (28.55) | 28 (100.0) |
Other results
Of the 28 cases assessed, only one prescription (for pneumonia) did not contain an antibiotic medication. Seventeen (60.7%) prescriptions contained one antibiotic medication, and ten (35.7%) contained two antibiotics prescriptions. Overall, five (17.9%) prescriptions contained one medication, 12 (42.9%) contained two medications, nine (32.1%) contained three medications, and two (7.1%) contained four medications.
DISCUSSION
This study was designed to determine the occurrence of lower respiratory tract infections (LRTIs) in the study setting and assess its management. The total occurrence of LRTIs at 8.6% out of 422 sampled cases is close to the findings from a study conducted in Botswana, where there were only 5.0% of pneumonia cases among RTIs presented in the primary health care setting.[16,18] These findings demonstrate the low occurrence of LRTIs when compared to upper respiratory tract infections (URTIs).[14,19] However, a study conducted in Ethiopia found an alarming 40.3% of LRTIs in the study setting.[20] The most prevalent LRTI in our study was pneumonia (71.4%), showing its dominance over other LRTIs such as bronchiolitis, the only other LRTI diagnosed in our study. Pneumonia is known as the most common LRTI in children and the only occurring LRTI in the Botswana study. However, a study conducted in Congo Brazzaville found bronchiolitis to be the most common LRTI in the study setting.[21] The prognosis of pneumonia can be poor if not treated according to guidelines.
The general approach to the management of LRTIs in our study setting was commendable, although not altogether in line with the guidelines of the Federal Ministry of Health and the pediatric association of Nigeria. Antibiotics were prescribed for all cases of bronchiolitis and all but one case of pneumonia. This shows inappropriate prescribing and management because bronchiolitis benefits from symptomatic management for relief rather than antibiotics since it is of viral origin. Antibiotics for bronchiolitis would only be appropriate if laboratory tests reveal the presence of bacteria as the causative organism.[7,22] The most prescribed antibiotics were cefuroxime and amoxicillin/clavulanate, indicating their preference over amoxicillin alone, as suggested by many findings, the WHO, and the pediatric association of Nigeria.[4,11,23,24] Also, in the WHO guidelines for the management of uncomplicated LRTIs in children, amoxicillin at a dose of 50 mg/kg/day in two divided doses or co-trimoxazole is recommended as the first-line agent at 8 mg/kg/day, in two divided doses.[25] Erythromycin and azithromycin, which are macrolides, were used alone or combined with cefuroxime or amoxicillin/clavulanate in our study. Although this is not in line with the standard treatment guidelines for Nigeria, some authors have reported that the use of macrolides is effective for community-acquired pneumonia (CAP), and it is included in the guidelines for the management of pneumonia by the pediatric association of Nigeria.[11,12,22] According to the pediatric association of Nigeria, other antibiotics prescribed, such as gentamicin, are given together with ceftriaxone, a combination reserved for severe pneumonia. While these may not have been in the standard treatment guidelines, prescribers tend to prescribe what they think would be effective.
Possible interactions that constitute drug therapy problems were suggested when some antibiotic combinations used in our study setting were checked on the Medscape Application Interaction Checker (MAIC). Combinations such as cefuroxime/azithromycin, cefuroxime/erythromycin, or amoxycillin/clavulanate were indicated to be associated with pharmacodynamic antagonism with bacteriostatic drugs like the macrolides interacting with the actions of the bactericidal drugs which can ultimately lead to treatment failure.[26] These practices, as posited by Periantoni and colleagues, emphasize nonadherence to established guidelines and, as a result, risk ineffective therapy and antimicrobial resistance.[7] Some reasons for nonadherence to guidelines are lack of time to educate parents, parental anxiety and/or pressure, and the need to retain patients.[27]
In the management of LRTIs in our study setting, we found that no test was conducted for 25 (89.3%) patients, which suggests that most of the patients were empirically managed. This agrees with the treatment guidelines of the pediatric association of Nigeria where it was surmised that for ambulatory patients with suspected community-acquired pneumonia, any form of investigation might not be necessary and has not been shown to impact the outcome of therapy when done.[11]
Of the children who presented with LRTI only, the majority (46.4%) were aged between one and eleven months, corroborating the findings of a study conducted in Zambia.[28] This finding may be because this age group still has a developing immunity and is yet to be exposed to certain immunization schedules that would protect them from LRTIs, or other predisposing reasons, such as the intake of complementary meals.[29]
Most (75%) of the prescriptions contained two to three medications, including antihistamines. Antibiotics (one or two) were also prescribed to all (96.4%), but one patient who had pneumonia.This conforms to the recommendations of the Revised WHO classification and treatment of childhood pneumonia at health facilities, where at least one antibiotic is recommended to manage pneumonia.[24]
Some adjunctive medications were also administered alongside antibiotics. The most administered (28.6%) supportive medication was ascorbic acid, which is widely known for its role in oxidative stress, wound healing, and immunity and in warding off pneumonia.[30,31] Cough syrups and antihistamines have been found to provide no benefits as adjunctive medication in CAP management.[11,27] Although the role of supplementation in disease trajectory is not beneficial in acute pneumonia, multiple studies have shown and agree that vitamin A can reduce mortality from all infective causes if used as preventive supplementation in children.[32]
CONCLUSION
The occurrence of LRTIs is low in our study setting, as expected. Although the management does not conform to Nigeria’s standard treatment guidelines, it broadly aligns with the recommendations of the WHO and the pediatric association of Nigeria. More studies need to be conducted to elucidate why physicians deviate from guidelines in Nigeria. However, it is important that the Federal Ministry of Health set up protocols or standard operating procedures according to acceptable guidelines in managing LRTIs in children at various levels of healthcare. The protocols will guide antibiotic use and prevent irrational prescribing to make the management of LRTIs in Nigeria nearly uniform. This will help quickly identify effective management to enable rapid consensual updates of established local guidelines when necessary.
Ethical approval
The research/study is approved by the Health Research and Ethics Committee of Alex Ekwueme Federal University Teaching Hospital, Abakaliki, number AE-FUTHA/REC/VOL 3/2022/008, dated 17th February 2022.
Declaration of patient consent
Patient’s consent is not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Acute lower respiratory infections among children under five in Sub-Saharan Africa: A scoping review of prevalence and risk factors. BMC Pediatr. 2023;23:225.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: A systematic analysis for the global burden of disease study 2015. Lancet. 2016;388:1459-544.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Changes in the epidemiology and burden of community-acquired pneumonia in Korea. Korean J Intern Med. 2014;29:735-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- 2023. Pneumonia In Children Factsheet. [accessed 2023 Aug 30]. Available from: https://www.who.int/news-room/fact-sheets/detail/pneumonia
- Childhood pneumonia at the University of Ilorin Teaching Hospital, Ilorin Nigeria. Niger J Paed. 2013;40:284-9.
- [Google Scholar]
- 2006. Pneumonia, the forgotten killer of children. [accessed 2023 Aug 31]. Available from: http://chromeextension://efaidnbmnnnibpcajpcglclefindmkaj/ https://factsforlife.org/pdf/Pneumonia_The_Forgotten_Killer_of_Children.pdf
- Antibiotic prescribing for lower respiratory tract infections and community-acquired pneumonia: An Italian pediatric emergency department’s real-life experience. Life. 2023;13:1922.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Appropriate antibiotic management of bacterial lower respiratory tract infections. F1000Res. 2018;7:F1000 Faculty Rev-1121.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Antibiotic misuse in respiratory tract infections in children and adults-a prospective, multicentre study (TAILORED Treatment) Eur J Clin Microbiol Infect. 2019;38:505-14.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Standard Treatment Guidelines (Second Edition). Abuja: Federal Ministry of Health, Abuja; 2016.
- Management of community acquired pneumonia (CAP) in children: Clinical practice guidelines by the Pediatric Association of Nigeria (PAN) Niger J Pediatr. 2020;49:210-39.
- [Google Scholar]
- Management of lower respiratory tract infection in outpatient settings: Focus on clarithromycin. Lung India. 2018;35:143-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Management of lower respiratory tract infection in outpatient settings: Focus on clarithromycin. Lung India. 2018;35:143-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pharmacological management of upper respiratory tract infections in children: An assessment of a tertiary institution practice in Nigeria. Am J Pharmacother Pharm Sci. 2023;2:13.
- [Google Scholar]
- Pathogens causing respiratory tract infections in children less than 5 years of age in Senegal. Microbiology Insights. 2019;12:1178636119890885.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Adherence to management guidelines in acute respiratory infections and diarrhoea in children under 5 years old in primary health care in Botswana. Int J Qual Health Care. 2005;17:221-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prescribing practices in the management of childhood diarrhoea in primary health care centres in a sub-urban community in Nigeria. Journal of Community and Primary Health Care. 2019;31:31-9.
- [Google Scholar]
- Childhood acute lower respiratory tract infections in northern Nigeria: At risk factors. Niger J Paed. 2015;42:188-93.
- [Google Scholar]
- Prevalence of acute respiratory infections among children under-five years old in a hospital in Port Harcourt, Nigeria: A two-year follow-up study. J Respir Med. 2018;2
- [Google Scholar]
- Acute lower respiratory tract infections and associated factors among under-five children visiting Wolaita Sodo University Teaching and Referral Hospital, Wolaita Sodo, Ethiopia. BMC Pediatr. 2021;21:413.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Child acute lower respiratory tract infection in pediatric intensive care unit at University Hospital of Brazzaville (Congo) Open J Pediatr. 2018;8:1.
- [Google Scholar]
- The management of community-acquired pneumonia in infants and children older than 3 months of age: Clinical oractice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2017;53:e25-e76.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Use of antibacterials in the management of symptoms of acute respiratory tract infections among children under five years in Gulu, Northern Uganda: Prevalence and determinants. PLoS ONE. 2020;15:e0235164.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Revised WHO classification and treatment of childhood pneumonia at health facilities. [accessed 2023 Aug 30] Available from: https://www.who.int/publications/i/item/9789241507813
- Lower respiratory tract infection in pediatrics, treatment approaches: Review article. Egypt J Hosp Med. 2018;73:6324-30.
- [Google Scholar]
- [accessed 2023 Aug 31]. Available form: https://reference.medscape.com/drug-interactionchecker
- Management of respiratory tract infections in young children-A qualitative study of primary care providers’ perspectives. NPJ Prim Care Resp Med. 2017;27:15.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Trends and factors associated with acute respiratory infection among under-five children in Zambia: Evidence from Zambia´s Demographic and Health Surveys (1996-2014) Pan Afr Med J. 2020;36:197.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Risk factors for acute respiratory tract infections in under-five children in Enugu Southeast Nigeria. Ann Med Health Sci Res. 2014;4:95-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Repositioning vitamin C as a promising option to alleviate complications associated with COVID-19. Infect Chemother. 2020;52:461-77.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Vitamin C and Infections. Nutrients. 2017;9:339.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Efficacy of zinc as adjunctive pneumonia treatment in children aged 2 to 60 months in low-income and middle-income countries: A systematic review and meta-analysis. BMJ Paediatr Open. 2020;4:e000662.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







