Translate this page into:
Functional Bracing for the Fracture Management in a Patient with Autism Spectrum Disorder- A Case Report
*Email: dr.aanshu@gmail.com
Abstract
Autism spectrum disorders affect behavior and alter personality of the affected individual to variable extent. The associated mental retardation and disinterested social interaction makes the treatment difficult. The fracture care in such patients is challenging and requires good understanding of the condition and that of patient. The involvement of family with active participation and supervised efforts are paramount in avoiding untoward complications. We highlight challenges of fracture care in one such adult female and effective role of functional bracing for a satisfactory outcome in selected cases.
Keywords
Autism
Autism Spectrum Disorder
Bone Density
Fracture Management
Humerus
Introduction
Autism Spectrum Disorders (ASD) is a developmental disorder involving abnormal communication and interaction within society along with other behavioral problems. These are also grouped as Pervasive Developmental Disorder (PDD). Its estimated reported incidence is about 1% of the population. Various kind of disorders are grouped under ASD and include autistic disorders, Asperger’s disorder and PDD not otherwise specified (PDD NOS)1. Usually diagnosed in early childhood, their presence is well recognized in adults. The bone density in patients affected with ASD has been found to be subnormal and decreased exercise and low vitamin D through diet or sun exposure might be additional causes for it2. The decreased bone mass may cause fractures but the literature regarding fracture in these cases is limited3. The treatment part is compounded with problems of social and behavioral disorders inherent to ASD.
Case Report
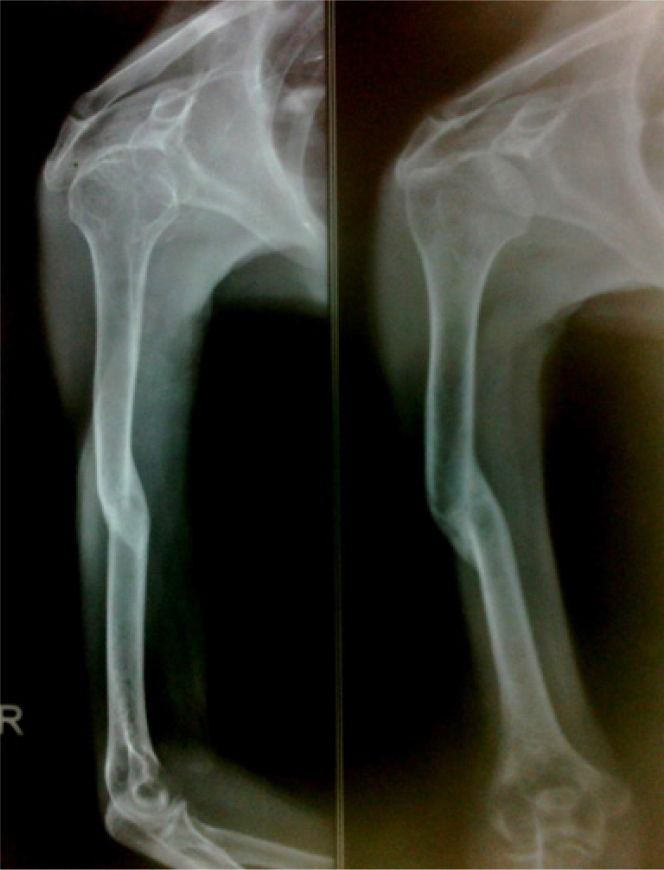
A28 year old female patient was brought to us with history of fall on wet bathroom floor and landing on her right arm. There was pain, deformity and disability in using the affected extremity since the injury. She was carried by her guardians with a sling of ‘dupatta’ (Indian stole). On examination visible deformity and abnormal mobility at middle of right arm was clinically suggestive of fracture. The distal neurovascular status was intact. The injury was closed and no remote or related injuries noted. The radiograph of the arm in orthogonal planes showed a short oblique mid shaft humerus fracture (Figure 1). The lady, according to history given by attendants was diagnosed case of autism and mental retardation. She was diagnosed in early childhood and initial workup and multiple opinions and treatment was taken with little clinical benefit. She is home bound as she has problem with socializing and communication. She was reluctant to visit anywhere for this injury as well and was somehow carried for treatment. The operative management and detailed investigation work up, as per standard protocol in our tertiary care referral centre, was declined by the patient and parents.

- The radiograph showing fracture of humerus shaft.
The treatment options were explained to the patient and family in detail. The cooperation of attendants and guardians was critical in the proper treatment in this case and they were informed about the procedure with pros and cons and potential pitfalls. The functional snug fitted coaptation ‘U’ cast of plaster of Paris was given and active movement of fingers advised. The plaster was evaluated in first week for loosening, breakage or tightness after three days and continued in the absence of any complications for three weeks (Figure 2). A second change of plaster cast was required for additional four weeks.

- The radiograph following application of functional plaster splint and showing uniting fracture.
Result
The fracture showed signs of union in the follow up radiograph and united well after two months of treatment. The union, however, was not anatomical but satisfactory with minimal shortening or angulations (Figure 3). No functional limitation was noted after short period of physiotherapy as patient resumed activities of daily living. No early or remote complication related to the fracture and technique was noted.
- The follow up radiograph showing united fracture.
Discussion
Low bone density has been attributed to increased risk of fractures and associated complications. The ASD cases have reportedly abnormal bone density thus increased risk for fractures4. Young and adult cases of ASD have been found to have an increased odds ratio of fracture around hip, forearm and spine3,5. Our case reported trivial fall resulting in a closed short oblique fracture pattern and that suggests subnormal bone strength6. Associated disorders related to mood and anxiety in cases with ASD is also commonly encountered. These coupled with social interaction issues create problem in the treatment of fractures7,8. There are ample reasons for non-compliance or adverse outcome of conservative outcome. The treatment opted by our case was conservative and conservative care requires periodic evaluation of radiographs and that of plaster or other splints to ensure adequacy and safety of the treatment. The additional feature of mental retardation in our case demanded cautious treatment option planning and vigilant support of attendants and guardians. With this background, we opted for functional bracing of the fracture right away as it will be least interfering and equally efficacious to the patient. The caution should be exercised to proactively evaluate for unsatisfactory displacement or complication of the conservative care all through the treatment period.
Conclusion
The management of fractures in the cases of autism spectrum disorder is challenging in many ways and judicious selection of treatment and supporting gesture of attendants is critical in satisfactory functional outcome.
Acknowledgement
None
References
- Brief report: Autism and Asperger syndrome in seven-year-old children: A total population study. J Autism Dev Disord. 1999;29:327-31.
- [CrossRef] [PubMed] [Google Scholar]
- Autism after adolescence: population-based 13-to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. J Autism Dev Disord. 2005;35:351-60.
- [CrossRef] [PubMed] [Google Scholar]
- Bone density in peripubertal boys with autism spectrum disorders. J Autism Dev Disord. 2013;43(7):1623-9.
- [CrossRef] [PubMed] [Google Scholar]
- Interim report and recommendations of the World Health Organization task-force for osteoporosis. Osteoporosis Int. 1999;10(4):259-64.
- [CrossRef] [PubMed] [Google Scholar]
- Reduced serum concentrations of 25-hydroxy vitamin D in children with autism: Relation to autoimmunity. J Neuroinflammation. 2012;9:201.
- [CrossRef] [PubMed] [Google Scholar]
- Brief report: Bone fractures in children and adults with autism spectrum disorders. J Autism Dev Disord. 2015;45(3):881-7.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome in adult life for more able individuals with autism or Asperger syndrome. Autism. 2000;4:63-83.
- [CrossRef] [Google Scholar]
- Psychiatric comorbidity of adults with autism spectrum disorders. Clin Neuropsychiatry. 2008;5:9-12.
- [Google Scholar]






