Translate this page into:
Frequency of Gestational Diabetes Mellitus in Pregnant Women Referred to Alavi Hospital in Ardabil, 2017
*Email: dr.shervin.tbn.@gmail.com
Abstract
Background:
Gestational Diabetes Mellitus (GDM) is the most common complications of pregnancy that spreading throughout the world and in the past 20 years has increased in range from 10% to 100% among racial groups. GDM cause to maternal and fetal side effects, and in the absence of treatment, it can cause macrosomia, respiratory distress, hypoglycemia, hypocalcemia, and hyperbilirubinemia in newborns.
Purpose:
The aim of this study was to investigate the frequency of GDM in pregnant women in Ardabil, Iran.
Method:
This retrospective cross-sectional study was conducted on 4485 pregnant women referred to Alavi hospital in Ardabil from April 2017 to December 2017. Data were extracted from hospital records and analyzed by statistical methods in SPSS version 16.
Results:
Of all Pregnant women, 256 (5.7%) had GDM. 91.7% of women with GDM had cesarean delivery which of them 75.5% were from urban and 73.2% were in the first parity. The mean age of women with cesarean delivery was 26.96 ± 6.38 years and normal delivery was 27.33 ± 6.44 years. Of women with GDM, 53% had primary education and most of them had no history of abortion and family history of diabetes.
Conclusion:
Considering the increased frequency of GDM in this study in compare with previous studies, the higher rate of cesarean section among young women with diabetes, doing more studies are essential in future.
Keywords
Ardabil
Gestational Diabetes Mellitus
Risk Factor
Screening
Introduction
GDM is defined as any degree of glucose intolerance, with onset and first recognition during pregnancy1. GDM is the most common metabolic disorder during pregnancy and its prevalence in different societies depends on strain and geographical location may range from 1% to 14% and in average included 4-5 % of all pregnancies in Iran and its prevalence in range 1.8-3.8 %2-6. GDM is one of the major risk factors for type 2 diabetes, and is more epidemiologically diagnosed with type 2 diabetes. About one third of women with type 2 diabetes had a history of GDM, and aging and body mass index are associated with GDM5,7-9. GDM is commonly associated with complications in mothers and infants and it is estimated that 90% of pregnancy problems such as preeclampsia, high mortality rates and having cesarean delivery are associated with GDM. Children born of mothers with GDM are also more likely to be exposed to obesity, glucose intolerance and diabetes in childhood and adulthood10-14. The increased prevalence is attributed to the aging population structure, urbanization, the obesity epidemic and physical inactivity1.
Age over 30 years old, high BMI and obesity, low activity, smoking, genetic disorders, previous GDM, family history of diabetes and history of abortion are known as effective risk factors in the prevalence of GDM. Older age is one of the risk factors for GDM, because by increasing the age, the risk of GDM was increased. Considering the importance of GDM and for prevent its complications in mother and infant, this study was conducted to investigate the frequency of GDM in women in Ardabil, Iran.
Materials and Methods
This retrospective cross-sectional study was conducted on 4485 pregnant women in 28-43 weeks of gestational age that referred to Alavi hospital in Ardabil city from April to December 2017. Data were collected from women hospital records, such as demographic information, family history of diabetes, abortion history, parity, gestational age, type of delivery and infants birth weight, and then analyzed by statistical methods in SPSS version 16. The p<0.05 was considered statistically significant. The design of study was approved by ethical committee of Ardabil University of Medical Science.
Results
Of all pregnant women, 256 (5.7%) had GDM that of them, 235 mothers (91.7%) had cesarean delivery. The prevalence of GDM among women with cesarean delivery was 11.4% and in normal delivery was 0.9%, and the difference was statistically significant. The mean age of women with CS was significantly lower than other women. 51.5% of women in aged 20-30 years had CS delivery, and the relationship between age and type of delivery was statistically significant (Figure 4). There was no significant difference between the mean weight of newborns born in cesarean and normal delivery. The highest gestational age was 43 weeks and at least 28 weeks and there was no significant difference between the mean of gestational age in cesarean and normal delivery (Table 1). Of women with GDM, 53% had primary education (Table 2). 75.5% of women in urban area and 57.1% in rural area had cesarean delivery, and the difference was not statistically significant (Figure 1). The most of mothers with normal delivery with 33.3% was seen in July and the most of CS with 18.3% was seen in June (Table 3). 73.2% of women with CS delivery had first parity and in more parities, the rate of normal delivery was significantly higher (Figure 2). Most diabetic women had no history of abortion and family history of diabetes, but there was a significant relationship between the history of abortion and type of delivery (Figure 3, Table 4). 50.8% of infants had birth weight between 2500 and 3500 gr but there was no relationship between the birth weight of newborns and the type of delivery in GDM women (Table 5). 51.5% of mothers with CS delivery were in the age group of 20-30 years (Figure 4).
| Variables | Type of delivery | p-value | |
|---|---|---|---|
| CS | Normal | ||
| Age of mother | 27±6.4 | 27.3±6.4 | 0.002 |
| Gestational age | 38.5±2.2 | 38.3±1.3 | 0.8 |
| Infant birth weight | 3472±55 | 3602±48 | 0.3 |
| Education | Type of delivery | Total | p-value | ||||
|---|---|---|---|---|---|---|---|
| CS | Normal | n | % | ||||
| n | % | n | % | ||||
| Illiterate | 10 | 4.3 | 2 | 9.5 | 12 | 4.7 | 0.68 |
| Beginner | 127 | 54 | 9 | 42.9 | 136 | 53.1 | |
| Diploma | 68 | 28.9 | 7 | 33.3 | 75 | 29.3 | |
| University | 30 | 12.8 | 3 | 14.3 | 33 | 12.9 | |
| Month | Type of delivery | Total | p-value | ||||
|---|---|---|---|---|---|---|---|
| CS | Normal | n | % | ||||
| n | % | n | % | ||||
| April | 27 | 11.5 | 2 | 9.5 | 29 | 11.3 | 0.36 |
| May | 33 | 14 | 1 | 4.8 | 34 | 13.3 | |
| June | 43 | 18.3 | 4 | 19 | 47 | 18.4 | |
| July | 42 | 17.9 | 7 | 33.3 | 49 | 19.1 | |
| Aguste | 25 | 10.6 | 2 | 9.5 | 27 | 10.5 | |
| September | 18 | 7.7 | 1 | 4.8 | 19 | 7.4 | |
| November | 23 | 9.8 | 4 | 19 | 27 | 10.5 | |
| December | 24 | 10.2 | 0 | 0 | 24 | 9.4 | |
| History of diabetes | Type of delivery | Total | p-value | ||||
|---|---|---|---|---|---|---|---|
| CS | Normal | n | % | ||||
| n | % | n | % | ||||
| + | 199 | 84.7 | 19 | 90.5 | 218 | 85.2 | 0.3 |
| - | 36 | 15.3 | 2 | 9.5 | 38 | 14.8 | |
| Birth weight | Type of delivery | Total | p-value | ||||
|---|---|---|---|---|---|---|---|
| CS | Normal | n | % | ||||
| n | % | n | % | ||||
| 2500> | 13 | 5.5 | 0 | 0 | 13 | 5.1 | 0.5 |
| 3500-2500 | 119 | 50.6 | 11 | 52.4 | 130 | 50.8 | |
| 4000-3500 | 70 | 29.8 | 8 | 38.1 | 78 | 30.5 | |
| 4000< | 33 | 14 | 2 | 9.5 | 35 | 13.7 | |

- Relation between residence place and type of delivery in diabetic women.
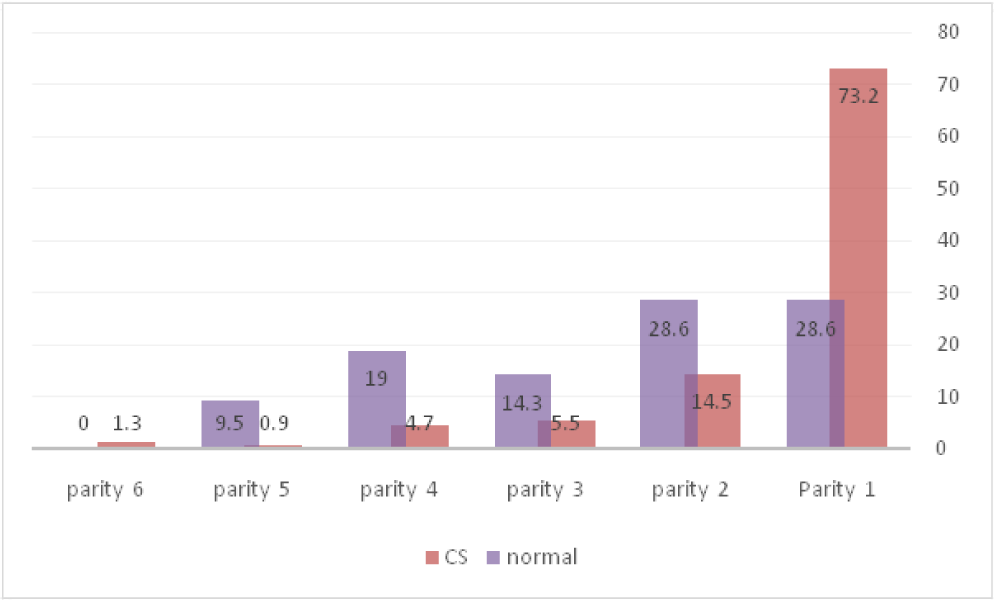
- Relation between parity and type of delivery in diabetic women.
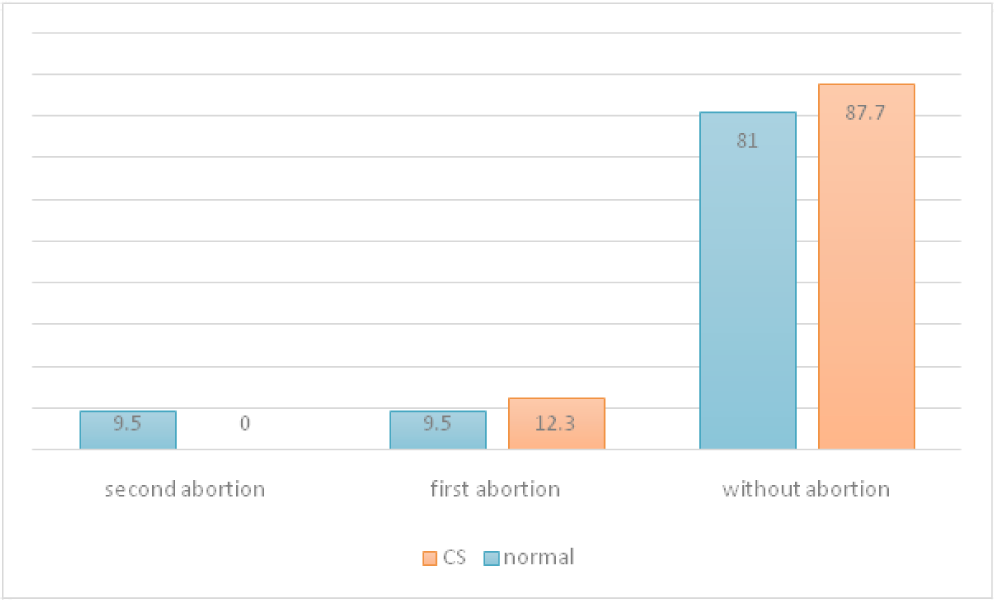
- Type of delivery by history of abortion in diabetic women.
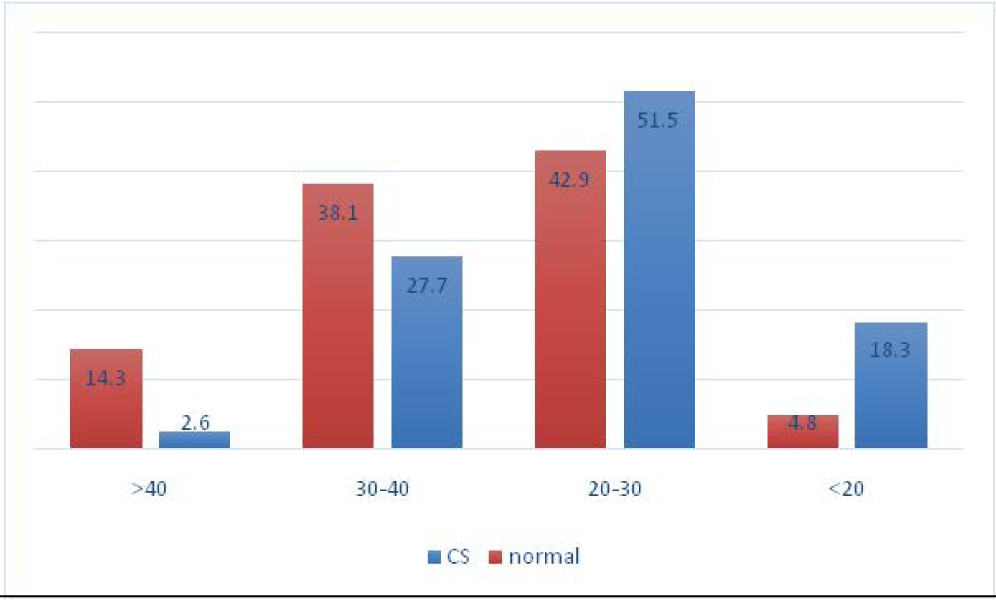
- Relation between age and type of delivery in diabetic women.
Discussion
GDM has a different prevalence due to racial differences in different parts of the world. In the United States and among native American, Asian and Spanish women, there was a higher risk of developing GDM than white women15. In Iran, in a review study of 1011 articles, the prevalence of GDM was 3.4% and in another study it was 4.9%. In other studies in Tehran, the prevalence of GDM was 4.6% and 2.4% in the north and northwest of the country. In the current study, the prevalence of GDM was 5.7%, which was slightly more than recent studies. The high prevalence of GDM in this study may be related to the more number of participants in the study, as well as the type and method of screening5,9,16-18. GDM is known as one of the causes of CS delivery. Studies have shown that the prevalence of CS among untreated diabetic women was higher than that of women with controlled diabetes. In this study, 91.7% of mothers with diabetic had CS delivery that most of them were women in aged 20-30 years with the first birth experience. In the study of Keshavarz et. al., the prevalence of CS delivery in diabetes women with more than 30 years old was 87.1% and in the study of Larijani et. al., the rate of cesarean section was 47.13% which was lower than our study. It seems that the higher rate of CS in age group 20-30 years in this study is due to complications associated with GDM, low support of the patients in normal vaginal delivery and low gestational age because by increasing age of mothers in the present study, the rate of delivery of cesarean section decreased and natural delivery increased4,10,16,19-22. In the present study the mean age of diabetic mothers was 27 years which was less than the average age reported in Chasan-Taber, Keshavarz, Bouzari et. al., and Ardabil study5,10,18. Family history of diabetes and abortion are the other risk factors for the GDM. In a review study in Iran, results showed that having a family history of diabetes increased the chance of getting GDM by 46.3%. In the present study, 14.8% of women had a family history of diabetes and 12.9% had a history of abortion which was less than similar studies for example, in the study of Larijani 33.33% of mothers had a family history of diabetes and 24.5% had a history of abortion and in the Ferrara study, the family history of diabetes was 47.3% which was higher than the present study9,22-25. The birth weight can be one of the predictors of the prediction of GDM relapses because women with a fetal macrosomia (4000 gr) had 40% higher probability of GDM relapse than women who had a baby between 3990-2500 gr. In the present study, 13.7% of newborns were over 4000 gr. The high birth weight of newborns in diabetic women can be one of the reasons for CS delivery and in a study, it was shown that in order to prevent a spinal cord injury in neonates with an estimated weight of 4,500 grams in diabetic mothers, 433 cesarean are needed at a cost of $930,000 but in this study, the mean weight of newborns between CS and normal delivery was not different13,18,25. In the present study, 50% of diabetic women had primary education, while in the study of Ferrara et. al., this rate was 16.7%, which was lower than our study results24. It was found that differences in screening programs and diagnostic criteria or various ethnic groups make it difficult to compare frequencies of GDM among various population26.
Conclusion
The results showed that the prevalence of GDM in pregnant women was slightly higher than recent studies in Iran and due to the high rate of CS among young women with diabetes, more studies are needed for study the reason for increasing the CS rate and the use of modern screening methods for identifying diabetic women and preventing the complications of GDM in mother and infants seems necessary.
References
- Prevalence of GDM in a medical college in South India : a pilot study. IJCP. 2014;25(4):342-47.
- [Google Scholar]
- International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676-82.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;2008(358):1991-2002.
- [Google Scholar]
- Elsevier. 2008. Available from: http://www.thelancet.com/journals/lancet/article/PIIS0140673608607333/fulltext
- [Google Scholar]
- Gestational diabetes: is it preventable? American Journal of Lifestyle Medicine. 2012;6(5):395-406.
- [CrossRef] [Google Scholar]
- Prevalence and risk factors of gestational diabetes in Iran: a systematic review and meta-analysis. Iran J Public Health. 2015;44(8):1036-44.
- [Google Scholar]
- Epidemiology of glucose intolerance and gestational diabetes in women of childbearing age. Diabetes Care. 1998;21(2):B9-13.
- [PubMed] [Google Scholar]
- Gestational diabetes mellitus: prevalence, risk factors, maternal and infant outcomes. Int J Gynaecol Obstet. 2001;75(3):221-8.
- [CrossRef] [PubMed] [Google Scholar]
- Insulin secretion and insulin resistance in pregnancy and GDM: implications for diagnosis and management. Diabetes. 1991;40(Suppl 2):18-24.
- [CrossRef] [PubMed] [Google Scholar]
- Gestational diabetes in Iran: incidence, risk factors and pregnancy outcomes. Diabetes Res Clin Pract. 2005;69(3):279-86.
- [CrossRef] [PubMed] [Google Scholar]
- Small size at birth and later diabetic pregnancy. Obstet Gynecol. 1998;92(5):781-4.
- [CrossRef] [PubMed] [Google Scholar]
- Screening for gestational diabetes mellitus in the subsequent pregnancy: Is it worthwhile? Am J Obstet Gynecol. 2002;187(4):918-21.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetes in pregnancy: a review of current evidence. Curr Opin Obstet Gynecol. 2007;19(6):586-90.
- [CrossRef] [PubMed] [Google Scholar]
- Management of Gestational Diabetes Mellitus. Am Fam Physician. 2003;68(9):1767-72.
- [PubMed] [Google Scholar]
- Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care. 2007;30(Suppl 2):S141-6.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of gestational diabetes in pregnant women referring to Ardabil health centers, 2003. Journal of Ardabil University of Medical Sciences. 2004;4(3):32-9.
- [Google Scholar]
- Prevalence of gestational diabetes mellitus in Iran: a systematic review and meta-analysis study. The Iranian Journal of Obstetrics. Gynecology and Infertility. 2013;15(40):16-23.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of gestational diabetes and its risk factors in pregnant women referred to health centers of Babol, Iran, from September 2010 to March 2012. The Iranian Journal of Obstetrics. Gynecology and Infertility. 2013;16(43):6-13.
- [Google Scholar]
- Cesarean delivery in relation to birth weight and gestational glucose tolerance: Pathophysiology or practice style? JAMA. 1996;275(15):1165-70.
- [CrossRef] [PubMed] [Google Scholar]
- The Hyperglycemia and Adverse Pregnancy Outcome Study. Associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012;35(4):780-6.
- [CrossRef] [PubMed] [Google Scholar]
- A review on the prevalence of gestational diabetes mellitus (GDM) in different regions of Iran. Journal of Diabetes and Metabolic Disorders. 2009;8:7.
- [Google Scholar]
- The prevalence of gestational diabetes mellitus in young women. Iranian Journal of Endocrinology and metabolism. 2002;4(1):23-7.
- [Google Scholar]
- Family history of diabetes and the risk of gestational diabetes mellitus in Iran: a systematic review and meta-analysis. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2017;11:S99-S104.
- [CrossRef] [PubMed] [Google Scholar]
- A pregnancy and postpartum lifestyle intervention in women with gestational diabetes mellitus reduces diabetes risk factors: a feasibility randomized control trial. Diabetes care. 2011;34(7):1519-25.
- [CrossRef] [PubMed] [Google Scholar]
- Rates and risk factors for recurrence of gestational diabetes. Diabetes care. 2001;24(4):659-62.
- [CrossRef] [PubMed] [Google Scholar]
- The Relationship between Some Risk Factors and Gestational Diabetes Mellitus in Pregnant Women Referred to Health and Treatment Centers in Zahedan, Iran, in 2012. IJHS. 2015;3(1):44-51.
- [Google Scholar]






